Virtual
Virtual Schedule at a Glance
Daily Raffle Drawing Time: 12:35 PM
All registered attendees (in-person and virtual) are automatically entered into the daily raffle.
FRIDAY, OCTOBER 6
7:45 AM
Attendee Log-in
7:00 AM –12:35 PM General Questions Email: Staff@cvma.net
Mark Epstein, DVM, DABVP (C/F), CVPP Topic: Pain Management
8:00 AM-9:00 AM
Trans Operative Pain Management for the Low-Surgical Dose Patient
9:05 AM-10:05 AM Trans Operative Pain Management for the High-Surgical Dose Patient
10:05 AM-10:30 AM 25-Minute Break
10:30 AM-11:30 AM Locoregional Anesthesia – Part 1
11:35 AM-12:35 PM
Locoregional Anesthesia – Part 2
SATURDAY, OCTOBER 7
7:45 AM
Attendee Log-in
7:00 AM –12:35 PM General Questions Email: Staff@cvma.net
Mark Epstein, DVM, DABVP (C/F), CVPP Topic: Pain Management
8:00 AM-9:00 AM Oral Medications for the Chronic Pain Management
9:05 AM-10:05 AM Parenteral Medications for the Chronic Pain Patient
Elizabeth Rozanski, DVM, DACVECC, DACVIM (SAIM) Topic: Emergency Critical Care | Respiratory Disease
10:05 AM-10:30 AM 25-Minute Break
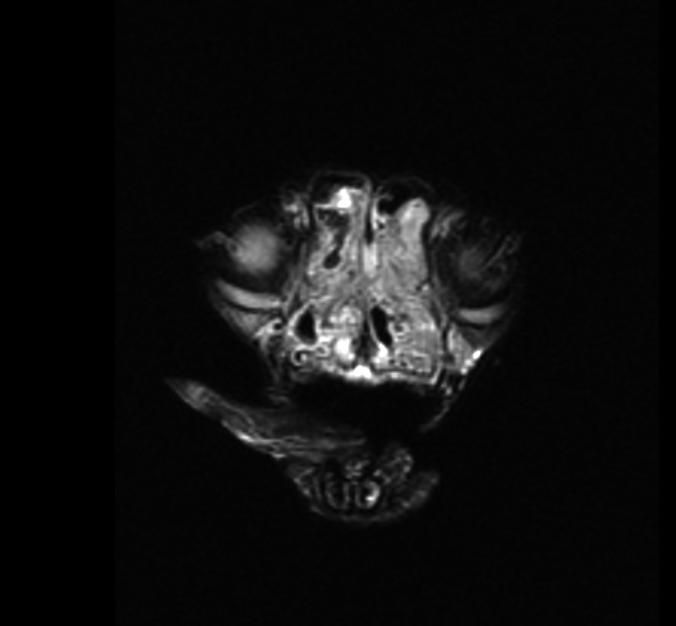
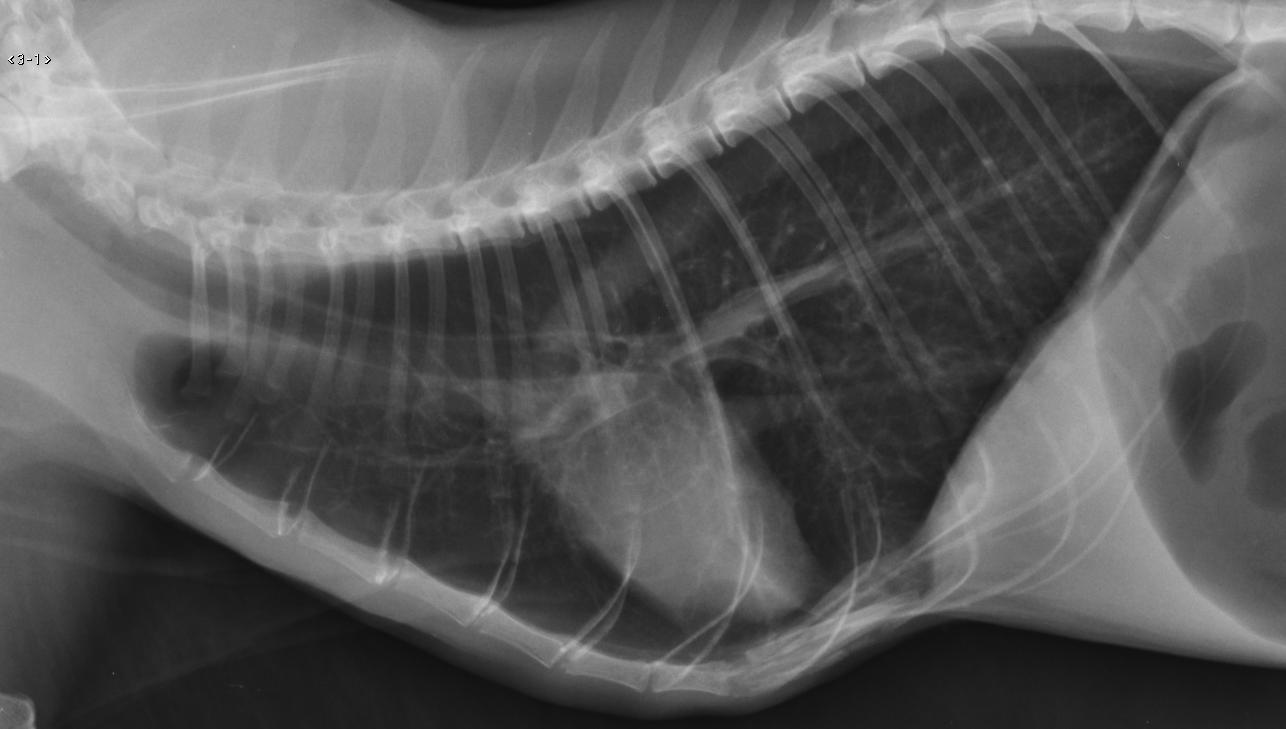
10:30 AM-11:30 AM Brachycephalics: The Worst Is Yet to Come
11:35 AM-12:35 PM Feline Respiratory Distress: It Is Not Always Bad!
SUNDAY, OCTOBER 8
7:45 AM Attendee Log-in
7:00 AM –12:35 PM General Questions Email: Staff@cvma.net
Elizabeth Rozanski, DVM, DACVECC, DACVIM (SAIM) Topic: Emergency Critical Care | Respiratory Disease
8:00 AM-9:00 AM The Airway Is Your Air-Emy
9:05 AM-10:05 AM The Geriatric Pet in the ER
10:05 AM-10:30 AM 25-Minute Break
10:30 AM-11:30 AM
Feline Trauma: How Are They Different?
11:35 AM-12:35 PM The Acute Abdomen
Thank you for attending this year’s CVMA Fall Seminar

Please take a few minutes to complete the on-line survey that will be emailed to you on Sunday. Your evaluation is extremely important to help us maintain and/or improve our conference quality!
CE Certificates will be emailed the week of October 9-13, 2023
Fall Seminar
October
CVMA
|
6-8, 2023
Speaker Biography
Mark Epstein, DVM, DABVP (C/F), CVPP
Dr. Mark Epstein received his DVM degree from the University of Georgia and is the senior partner and medical director of TotalBond Veterinary Hospitals, a small group of AAHA-accredited practices in North Carolina. He is a diplomate and pastpresident of the American Board of Veterinary Practitioners (ABVP) (Canine/Feline). Dr. Epstein is certified by the Academy of Integrative Pain Management (AIPM), is recognized as a Certified Veterinary Pain Practitioner (CVPP) by the International Veterinary Academy of Pain Management (IVAPM), and is a past-president of IVAPM. He is currently President of the IVAPM Research and Scholarship Foundation. Dr. Epstein chaired the AAHA Senior Care Guidelines Task Force and co-chaired the 2015 AAHA/AAFP Pain Management Guidelines Task Force. He is a recipient of the 2022 Viticus Group Small Animal Educator of the Year Award.

CVMA Fall Seminar- October 6-8, 2023
Dr. Mark Epstein
Trans Operative
Pain Management for the
Low-Surgical Dose Patient
1
Trans Operative Pain Management for The Low-Surgical Dose Patient
Mark E. Epstein, DVM, DABVP (C/F), CVPP TotalBond Veterinary Hospitals, PC Gastonia, Charlotte NC, Lake Wylie SC
The robust advances in pain management for companion animals underlie the decision of AAHA and AAFP to expand on the information provided in the 2007 AAHA/AAFP Pain Management Guidelines for Dogs and Cats. The 2015 Guidelines can be found at these URL’s: http://jfm.sagepub.com/content/17/3/251.full.pdf+html https://www.aaha.org/globalassets/02-guidelines/2022-pain-management/resources/2022-aaha-pain-management-guidelinesfor-dog-and-cats_updated_060622.pdf and), and the 2022 AAHA.
Guidelines can be found at 2022 AAHA Pain Management Guidelines for Dogs and Cats
The Guidelines continue the trend in all branches of medicine toward evidence-based consensus statements that address key issues in clinical practice. Although not a review article, the Guidelines represent a force multiplier for the busy practitioner, consolidating in a single place current recommendations and insights from experts in pain management. The recommendations of the guidelines Task Force are evidence based insofar as possible and otherwise represent a consensus of expert opinion. These notes contain the key applied principals for veterinary clinicians.
Devising an evidence-based top-tier trans-operative pain management strategy is within the scope of any practice to achieve. The framework of effective pain management systems rests solidly on the foundation of recognition/assessment, pre-emption, and using multiple modalities. Multiple modalities allow for intervention at several different places of the nociceptive pathway, increasing effectiveness and minimizing the need for high or protracted doses of any one particular drug (including, perhaps especially, opioids), and minimizes the likelihood or severity of peripheral and central sensitization which contributes to maladaptive (exaggerated) pain. Veterinary medicine would do well to emulate a recent trend in human trans operative care called ERAS – Enhanced Recovery After Surgery, a which aims for evidence-based measures to 1. Reduce Surgical stress, 2. Maintain physiologic functions, and 3. Enhance mobilization after Sx; outcomes measured include: 1. Reduced morbidity rates, 2. Faster recovery, 3. Shorter hospital stays. Chief among the strategies to achieve the ERAS goals is to minimize the minimization of opioid use. 1
The basic construct for low-surgical dose patients is a 4-legged stool:
1.ANXIOLYTICS
Anxiety contributes directly to the hyperalgesic state through cholecystkinin-mediated “nocebo” effect. 2 A number of studies in humans support the idea that patients who are highly anxious or stressed pre-operatively experience higher pain scores post-operatively. These observations are also found in many animals studies, where restraint, social defeat, rotation – all things veterinary patients experience in the normal pre-surgical setting in order to draw blood, place catheters, etc. – contribute to hyperalgesia. 3
Thus, the first leg of a strong transoperative pain management protocol does not involve the use of analgesics in and of themselves, but anxiolytics and not just pharmacologic ones i.e. low-stress handling techniques, b the Fear Free™, c experience to include (but not limited to) pheromones and addition to tranquilizers/sedatives such as trazodone (8-
a https://erassociety.org/
b http://drsophiayin.com/lowstress, http://www.catvets.com/guidelines/practice-guidelines/handling-guidelines
c https://fearfreepets.com/
2
10mg/kg) or gabapentin (15 mg/kg) for the owner to administer at home pre-visit. In hospital, clinicians may choose between phenothiazines (e.g. acepromazine), benzodiazepines (midazolam or diazepam), or alpha2 agonists (dex/medetomidine).
2.OPIOIDS
Opioid receptors are distributed ubiquitously throughout the body and can be found in most central and peripheral tissues. Several opioid different receptor types and subtypes have been isolated, each with a variant effect; activation of an opioid receptor inhibits presynaptic release and postsynaptic response to excitatory neurotransmitters. The proposed mechanism includes opioid receptor coupling with the membrane-associated G protein; this leads to decreased intracellular formation of cAMP which diminishes calcium channel phosphorylation (closing off the channel) and opens potassium channels enhancing potassium influx. The resulting effect is hyperpolarization of the neuron and blockade of Substance P release. Nociceptive transmission is thus greatly impeded. Opioids in combination with anxiolytics discussed above can induce a profound sedating Neuroleptanalgesic effect to the patient’s benefit. However, recent efforts to reduce the frequency, duration, and dosing of full mu agonists (e.g. morphine, hydromorphone, fentanyl) in favor (while still maintaining patient comfort) of partial mu agonists (buprenorphine) and mu-antagonist/kappa agonist (butorphanol) in human medicine are being mirrored in the veterinary profession https://ivapm.org/wp-content/uploads/2018/12/Op-Sparring-Task-Force-WP.pdf.
Different opioid drugs are available which vary in their relative potency and receptor affinity, and a complete discussion of their similarities and differences are available in a number of resources. Full-mu agonists have the most significant analgesic punch, but in low-surgical dose patients it can be argued should be used only short-term (e.g. hydromorphone as a pre-medication). Full mu agonists do not have a ceiling effect which means higher doses can achieve more profound analgesic but with accompanying increases in adverse effects (dysphoria, suppressed appetite and in the extreme constipation, hyperalgesia, and potentially fatal respiratory suppression however uncommon this might be in animals). Recognizing and having strategies for counteracting their signs will minimize the complications that they present. 4
Buprenorphine is a partial mu agonist so less potent an analgesic than full mu agonists and can be considered suitable for low-surgical dose patients. It has a ceiling effect, meaning higher doses elicit neither additional analgesia nor much more in the way of adverse effect. Buprenorphine does have a higher affinity for the mu receptor than full mu agonists and will displace those molecules if both are present. Buprenorphine also has the unique feature of taking significant time to achieve maximum effect (1-hour IM, 30 min IV); and it is the least sedating of commonly used opioids in veterinary medicine.
Butorphanol is a mu agonist and a kappa antagonist; like buprenorphine it has a ceiling effect. However, its short duration of action in the dog (approx. 30-40 min) generally makes it a poor choice for surgical analgesia in this species, although co-administered with alpha-2 agonists (e.g. dexmedetomidine) it will act syngergistically for both pain and sedation and this combination can be appropriate for low-surgical dose procedures.
Tramadol, in contradistinction to humans, does has negligible opioid activity in the dog, but cats have opioid (and serotonin, norepinephrine) metabolites similar to humans.
3.NSAID
The primary mode of action is to inhibit cyclooxygenase 2 (COX2), the enzyme that is expressed at site of inflammation and results in the production of pro-inflammatory and vasoactive prostaglandins. Also, through poorly understood mechanisms, likely by modulating multiple gene expression pathways, 5 it may inhibit central perception of pain. Several superior products are now labeled for use in dogs and cats (meloxicam and robenacoxib are metabolized through oxidative rather than glucuronidase pathways), making them among the most popular of pain management medications in veterinary medicine. Pre-operative use of NSAID appears to be safe in healthy dogs
3
(even in the face of modest hypotension; but hypotension should be avoided with the use of IV fluids and careful blood pressure monitoring); robenacoxib is specifically labeled for pre-op use. However, it is satisfactory to administer post-operatively should that be the clinician’s preference. The adverse event profile however is wellestablished and results from metabolites of COX1 metabolism (especially in the GI tract), and also PGE2 from COX2 metabolism (especially in the renal tubules) do have normal homeostatic, tissue-protective, and tissue-healing effects. However, the frequency and severity of NSAID ADE can be minimized through well-established means. The GI and renal adverse effects can be expected to occur most commonly in higher risk patients, e.g.: hypovolemia, hypotension (including anesthetic procedures especially those not supported by intravenous fluids), pre-existing GI or renal disease, over usage, and the inappropriate combination with other NSAID’s or corticosteroids. Notable in this last category is client use of aspirin in their pets, which may be unbeknownst to the clinician unless specifically queried in a thorough history (uniquely, this NSAID produces a cyto-protective lipoxin through the COX pathway; 6 thus when COX is inhibited through the use of another, concurrently-given NSAID, the potential for GI toxicity is considerably enhanced) The very rare hepatic issues are idiosyncratic reactions of that dog to that molecule, and cannot be prevented or predicted based on liver enzymes (do avoid in liver dysfunction however).
Grapiprant is not COX-inhibiting but rather antagonizes just the EP4-receptor of PGE2 (responsible for activating nociceptors), sparing the EP1, EP2, EP3 subunits largely concerned with normal tissue function and repair.
Galliprant™ is labeled for osteoarthritis in dogs, and its use in acute, post-surgical pain remains to be determined (conflicting data as of this writing).
Robenacoxib (Onsior™, Elanco) has been approved for 3 days of post-operative pain relief in cats. It is COX2-selective with the unique feature of having a very short plasma elimination half-life of 1.7 hours (compared to meloxicam at approx. 20 hours), yet (because it like all NSAID is highly protein-bound) stays at the site inflammation/effusion for >24 hours. It is presumed that this novel PK profile lends itself to impressive safety data including up to 5 & 10X labeled dose. 7
4. LOCOREGIONAL ANESTHESIA
Local anesthetics were once a mainstay of pain management in veterinary medicine, and may now be one of the most under-utilized modalities. Administered locally or regionally, they are the only modality that renders complete anesthesia to a site, i.e. no transmission of nociceptive impulses as long as the drug exerts its effect. Initially used as a means of desensitizing tissues in order to “invade” tissues with scalpels; local anesthetics are enjoying a rebirth as powerful tools to prevent or reduce perioperative pain (as well as procedural and even chronic pain) and to reduce general anesthetic and concurrent analgesic (especially systemic opioid) requirements. There is no longer a reason to hold an “either-or” position; “for surgery either I use local anesthetics or I use general anesthesia”, in fact, there are many reasons to combine general and local anesthetic for surgical pain relief. 8 Simple techniques for the lowsurgical dose patients include: topical/dermal/epidermal local anesthetics for IV catheter placement (e.g. EMLA®, LMX4®, or their generic equivalents), incisional line blocks, field blocks for lumpectomies or laceration repairs, intraabdominal (peritoneal) blocks before laparotomy closure, orofacial blocks for extractions and mesovarium and intratesticular blocks for spay and neuter respectively, are well described in the literature.
4
1 Echeverria-Villalobos M, Stoicea N, Todeschini AB, Fiorda-Diaz J, Uribe AA, Weaver T, Bergese SD. Enhanced Recovery After Surgery (ERAS): A Perspective Review of Postoperative Pain Management Under ERAS Pathways and Its Role on Opioid Crisis in the United States. Clin J Pain. 2020 Mar;36(3):219-226.
2 Benedetti F, et al. The biochemical and neuroendocrine bases of the hyperalgesic nocebo effect, J Neruosci 2006 Nov 15;26(46):12014-22, IASP Pain Clinical Updates XV:1 March 2007
3 Martenson ME, Cetas JS, Heinricher MM A possible neural basis for stress-induced hyperalgesia. Pain 142 (2009): 236-244
4 Carr, DB (Ed.) Opioid Side Effects, In: IASP Pain Clinical Updates, April 2007 XV:2
5 Xiao-Min W et al Rofecoxib modulates multiple gene expression pathways in a clinical model of acute inflammatory pain, Pain 128(1-2) March 2007: 136-147
6 Schottelius AJ, Giesen C, et al. An aspirin-triggered lipoxin A4 stable analog displays a unique topical anti-inflammatory profile. J Immunol. December 2002;169(12):7063-70.
7 King JN, Hotz R, Reagen EL, Roth DR, Lees WS. Safety of oral robenacoxib in the cat. J Vet Pharmacol Ther. 2012 Jun;35(3):290-300.
8 Jones RS. Combining local and general anesthesia for better pain relief in dogs and cats. Vet J. 2008 Nov. 178(2):161-2
5
Trans Operative Pain Management for the High-Surgical Dose Patient
6
Trans Operative Pain Management for the High-Surgical Dose Patient
Mark E. Epstein, DVM, DABVP (C/F), CVPP TotalBond Veterinary Hospitals, PC Gastonia, Charlotte NC, Lake Wylie SC
Industry Pain Management Guidelines include:
2014 & 2022 WSAVA Global Pain Council: https://wsava.org/Global-Guidelines/Global-Pain-CouncilGuidelines/
2015 & 2022 AAHA
• http://jfm.sagepub.com/content/17/3/251.full.pdf+html
• https://www.aaha.org/aaha-guidelines/2022-aaha-pain-management-guidelines-for-dogs-andcats/home/
The Guidelines continue the trend in all branches of medicine toward evidence-based consensus statements that address key issues in clinical practice, and represent a force multiplier for the busy practitioner, consolidating in a single place current recommendations and insights from experts in pain management. The recommendations of the guidelines Task Force are evidence based insofar as possible and otherwise represent a consensus of expert opinion. These notes contain the key applied principals for veterinary clinicians.
Devising an evidence-based top-tier trans-operative pain management strategy is within the scope of any practice to achieve. The framework of effective pain management systems rests solidly on the foundation of recognition/assessment, pre-emption, and using multiple modalities. Multiple modalities allow for intervention at several different places of the nociceptive pathway, increasing effectiveness and minimizing the need for high or protracted doses of any one particular drug (including, perhaps especially, opioids), and minimizes the likelihood or severity of peripheral and central sensitization which contributes to maladaptive (exaggerated) pain. Veterinary medicine would do well to emulate a recent trend in human transportive care called ERAS – Enhanced Recovery After Surgery, a which aims for evidence-based measures to 1. Reduce Surgical stress, 2. Maintain physiologic functions, and 3. Enhance mobilization after Sx; outcomes measured include: 1. Reduced morbidity rates, 2. Faster recovery, 3. Shorter hospital stays. Chief among the strategies to achieve the ERAS goals is to minimize the minimization of opioid use. 1
The basic construct is a 4-legged stool even for Low-Surgical Dose Patients (covered in that session) include
• ANXIOLYTICS (pharmacologic, non-pharmacologic)
• OPIOIDS (short action, duration)
• NSAID
• LOCOREGIONAL ANESTHESIA
a https://erassociety.org/
7
High-Surgical Dose Patients can be defined as those undergoing procedures with existing evidence of, or significant risk factors for, hypersensitization, i.e. for post-surgical pain that includes pain exaggerated in scope, severity, duration, character, and field. This maladaptive pain experience can be said to be “Pain with a Neuropathic Component” and contribute significant to patient morbidity, delayed recovery, and in the extreme with patients on the edge, post-op mortality.
Patients with or at risk for maladaptive pain processing include but are not limited to those with:
1. Significant tissue trauma (orthopedic or soft-tissue; pre-existing, surgical, or both)
2. Pre-existing chronic inflammation
3. Nerve injury (pre-existing, surgical i.e. amputation, or both)
4. Any pre-existing chronic pain syndrome or having risk factors for peripheral neuropathy e.g. diabetes mellitus, vinca alkaloid chemotherapy
Such High Surgical Dose Patients require the same components, albeit somewhat amended, as Low Surgical Dose Patients, but also several more i.e. a 5-, 6-, sometimes 7- or 8-legged stool. These interventions may include one or more of the following:
Alpha-2 agonist: Medetomidine and dexmedetomidine binds opioid-like receptors on C- and A-delta fibers, especially in the central nervous system. Binding pre-synaptically, NE production is reduced and sedation occurs; binding post-synaptically, analgesia is produced, and is profoundly synergistic with opioids. It also blocks NE receptors on blood vessels, resulting in vasoconstriction; the resulting hypertension parasympathetically induces bradycardia, which is extended by a subsequent direct decrease in sympathetic tone. However, central perfusion is maintained and the author has found a wide use for these alpha-2 agonists in acute and peri-operative setting, though only in combination with opioids and at doses much lower than suggested by the manufacturer. One particularly novel and userfriendly utility is IV micro-doses intra- and post-operatively, 0.25 – 1.0 mcg/kg. This may result in intravenous volumes of only 0.01 – 0.03 ml in even the largest of dogs. Alpha-2 agonists can be administered safely in appropriate patients at a Constant Rate Infusion of 1.0 mcg/kg/hr (1.0 ml = 0.5 mg)/L administered at maintenance rate of 2 ml/kg/hr. 2
Zenalpha® is a new product that combines medetomidine + the peripheral alpha-2 antagonist vatinoxan. The product is labeled for IM sedation as a solo agent in dogs only, and attenuates medetomidine’s peripheral vasoconstriction which in turn attenuates the rise in peripheral vascular resistance, reflex bradycardia and drop in cardiac output. Extralabel usage over lower doses in combination with opioids, and administered intravenously, have been explored but ideal dosing has not been determined. It appears that atipamezole can be safely administered to further reverse the effects of Zenalpha® (but unlike the vatinoxan it includes, will also reverse the central (sedation, analgesic) effects as well. 3
Sub-anesthetic Ketamine CRI: A phencyclidine dissociative anesthetic, the evidence is building for its preemptive and preventive effects when given at subanesthetic doses in an intravenous constant rate infusion.
Ketamine binds to a phencyclidine receptor inside the NMDA receptor, i.e. the calcium channel would already have to be open and active for ketamine to exert its effect. However, once bound, it decreases the channel’s opening time and frequency, thus reducing Ca+ ion influx and dampening secondary intracellular signaling cascades. Hence it is unlikely (and has not been shown) to be truly analgesic in
8
nature. Rather, it appears to be protective against hyperalgesia and central hypersensitization in the post-operative setting, 4 including in the dog. 5 Ideal sub-anesthetic ketamine plasma concentrations –eliciting the most benefit with the least adverse effect – has been reported at 2-3 mcg/ml, which can be achieved by administering ketamine IV CRI at 10 mcg/kg/min. 6 This can be accomplished by placing 60 mg (0.6 ml of 100 mg/ml stock) ketamine in 1 L of fluids and administered at customary intra-operative rates of 10 ml/kg/hr. Post-operatively, the rate can be reduced to customary maintenance rates of 2 ml/kg/hr, which administers the ketamine CRI at 2 mcg/kg/min. A loading dose of 0.25 – 0.5 mg/kg ketamine IV is recommended prior to the initiation of the CRI in order to rapidly achieve plasma levels (can be achieved through ketamine itself, a “ketofol” mixture with reduced doses of propofol, ketamine/valium or Telazol™ induction). Human consensus guidelines advise that sub-anesthetic ketamine CRI should be deployed in patients undergoing more painful procedures, guidance that can be extrapolated to both dogs and cats; additionally, clinicians should consider utilizing this modality in patients with pre-existing chronic inflammation and known or suspected nerve injury.
Lidocaine CRI: The mechanisms behind a pain-modifying effect of systemic lidocaine remain an area of investigation but appear to include its ability to enter the nociceptor cell body in the dorsal root ganglion. In humans the evidence is strong for safety and the beneficial effects of intravenous lidocaine (IVL) on pain after abdominal surgery in humans (especially for the 1st 24 hours, and less so for other surgeries eliciting somatic pain) 7 , 8 , 9 , 10 and possibly horses, including both pain and return of bowel function.
Systemic, intravenous infusion of lidocaine has also been shown to elicit a sustained effect on neuropathic pain in humans. 11 Several systemic lidocaine CRI protocols are described, some combined with other pain-modifying agents. A customary one is described 12: 300 mg lidocaine 2% (15 ml) is placed in a liter of crystalloids, and administered at a surgical rate of 5-10 ml/kg/hr, delivering 25-50 mcg/kg/min. Postoperatively the rate may be reduced to maintenance rate of 2 ml/kg/hr, delivering 10 mcg/kg/min. Note: for accurate dosing, 15 ml of the crystalloid should be removed prior to the addition of the lidocaine. Lidocaine should be used with caution in hypovolemic states, and is advised for use in dogs only.
NSAID: Special Considerations.
Suppressing COX enzymes suppresses production of PGE2 and its pro-nociceptive, pro-inflammatory properties, but this molecule also promotes tissue healing through vasodilation and other means.
Fracture repair: Rodent and canine models reveal that NSAIDs elicit a time- and dose-dependent delay in fracture healing. 13 However the effect is reversible upon withdrawal of NSAID 14 and a human Metaanalysis (and FDA FOI data for veterinary-approved NSAIDs) do not support a clinically-relevant effect of delayed- or non-union fracture repair with judicious use of NSAIDs. It is generally considered not only safe, but appropriate to use NSAIDs post-fracture repair (including TPLO), but for a time period of days to weeks rather than months. One canine study showed no difference in radiographic healing between dogs without carprofen and those with 2-week administration of carprofen. 15
GI surgery: data in humans undergoing intestinal resection/anastomosis reveal a higher rate of leakage from the anastomotic site in cohorts receiving NSAID than those that do not. 16 There is not a clear consensus in veterinary medicine about NSAIDs use post-GI surgery is appropriate in dogs and cats. The author supports the use of NSAIDs in GI surgery as long as the bowel is healthy and patient not otherwise compromised, for the 1st 24-48 hours post-op.
9
Opioid: Use of extended-duration formulations:
In cats, Simbadol™ (Zoetis) is a 1.8 mg/ml buprenorphine FDA-approved product labeled for 24 hours of post-surgical analgesia in cats labeled for use at 0.24 mg/kg SC; the author utilizes a reduced dose of 0.12 mg/kg to minimize the modest adverse effects of lethargy and diminished appetite (and supported by more recent PK data although with wider range variability than the labeled dose 17). One recent study in dogs found the off-label use of Simbadol™ in this species at 0.02 mg/kg to be non-inferior to a 0.3 mg/ml product administered SC. 18
Newer on the market just in 2022 is Zorbium™ (Elanco), a transdermal buprenorphine product for cats. Placed on the skin between the shoulder blades, the product enters into the stratum corneum of the skin, resides there and slowly releases into systemic circulation from there providing 4 days of post-operative analgesia.
Enhanced-duration local anesthetic: Liposome-Encapsulated Bupivacaine
In 2016, an extended-release, LE-encapsulated bupivacaine product was FDA-approved for dogs undergoing stifle surgery (Nocita™, Aratana, since purchased by Elanco), eliciting 3-days of analgesic effect; in 2018 the label was extended to nerve block for digit surgery (onychectomy) in cats. The product has been available for several years in humans under the trade name Experel™. As the liposomes degrade, bupivacaine is released into the surrounding tissue, rendering its local anesthetic effect. The product itself is viscous and does not readily diffuse, therefore the label calls for utilizing an “advancing needle” technique whereby the product is deposited by repeat injections into the affected tissue, at each layer upon closure. A number of extra label uses have been described.
Maropitant (Cerenia®) is a central antiemetic through blockade of Substance-P to the NK-1 receptor, which is also involved in pain processing especially involving central sensitization. The true painmodifying effect in dogs remains uncertain. A 2020 Systematic Review of its use in dogs and cats revealed that the available evidence supports that it significantly reduces the minimum alveolar concentrations for gas anesthetic for many different surgical procedures, but that it had no clearly proven effect on inflammation and pain. 19 However, these were almost exclusively on ovariohysterectomy models which would generally not be expected to elicit central sensitization. Indeed, one study in a population of dogs with risk factors for hypersensitization (undergoing large soft tissue resection i.e. mastectomies), coadministration of maropitant IV (bolus followed by CRI) maropitant with ketamine and lidocaine CRIs had an adjuvant effect with minimal cardiorespiratory effects and effective analgesia, improving pain management and patient comfort. 20 Maropitant performed poorly in development as pain-modifying agent in humans and was withdrawn as a study target. However, the prospect remains it may provide benefit in a subset of patients (e.g. for visceral pain, with central sensitization) or with improved delivery systems (e.g. in a nanoparticle formulation). 21
Adjunctive drugs:
Tramadol: In humans, tramadol is described as a synthetic opioid with 1/100th of the affinity for the mu receptor as morphine but a much better analgesic effect than this would predict. This is likely due to the combined effect of a highly active M1 metabolite and serotonin- and norepinephrine (inhibitory neurotransmitters) agonism. However, recent work demonstrates that it appears to have a very short half-life (1.7 hours) in the dog, 22 and it appears that dogs produce very little of the M1 opioid
10
metabolite. 23 The unfavorable PK profile of oral tramadol in dogs, and in a Systematic Review and MetaAnalysis the lack of evidence to support a post-surgical pain-modifying effect 24 should lend skepticism about its use as an analgesic in this species. Cats do make the M1 metabolite in similar quantities and PK as humans, 25 and there are data to support its use for post-surgical pain in this species 26. Its bitter taste may limit its use in cats, but there are case reports and anecdotes of finding palatable versions in beef and marshmallow flavoring.
Gabapentin is labeled for use as an anti-convulsant drug but is in widespread human use for its analgesic properties. While structurally similar to GABA, it is not a direct agonist, although it may have indirect effects on GABA metabolism such as increasing intracellular stores. Another leading hypothesis is that it exerts effect through interaction with the alpha-2-delta subunit of the voltage gated calcium channel. 27 Its utility in chronic, neuropathic pain states is well-established in humans, 28 but more recently its utility in the transoperative setting is supported by a number of systematic reviews. 29 , 30 , 31 , 32 , 33 , 34
Pharmacokinetic studies in dogs reveal that it may have a half-life of 3-4 hours in the dog 35, suggesting a TID administration schedule. Based on experience in humans, pre-operative doses are recommended in the 10-15mg/kg mg/kg range and post-op 7-10 mg/kg 36. The primary adverse effect in dogs appears to be somnolescence (as in humans) which usually will spontaneously resolve over a few days’ acclimation time, but this AE not been a frequent occurrence in the author’s experience.
Acetaminophen (paracetamol, APAP) has an unidentified certain mechanism of action although may be predominantly by inhibiting a variant of COX1 in the brain, and bind to cannabinoid receptors. Although anecdotes and older studies may imply a pain-modifying effect, newer studies demonstrate that in the dog, oral (or suppository) APAP does not achieve serum levels generally associated with a pain-modifying effect. 37 However, acceptance of acetaminophen’s safety and potential analgesic and anti-pyretic in dogs effect appears to be growing. 38 The clinical benefit of administering a combined acetaminophen + oral opioid in dogs appears to be mixed at best with treatment failures high post-TPLO utilizing APAP+ hydrocodone, 39 and an inferior effect of APAP + codeine to standard NSAD in an model of acute inflammation. 40 This is likely due at least in part to the large first pass effect oral opioid in dogs compared to humans (therefore limiting its bioavailability). Note that prescribing oral opioid in any formulation puts these tablets into the public sphere, at risk for diversion and thus contributing to the opioid epidemic.
Non-pharmacologic interventions:
Cold-compression: Long known for its pain-modifying effect in humans, recent studies affirm a similar effect in dogs. 41 , 42
Therapeutic Laser: Two studies demonstrate a positive pain-modifying effect pre 43 - and post 44operatively, with one not improving better than placebo. 45
1 Echeverria-Villalobos M, Stoicea N, Todeschini AB, Fiorda-Diaz J, Uribe AA, Weaver T, Bergese SD. Enhanced Recovery After Surgery (ERAS): A Perspective Review of Postoperative Pain Management Under ERAS Pathways and Its Role on Opioid Crisis in the United States. Clin J Pain. 2020 Mar;36(3):219-226.
2 Lin GY, Robben JH, Murrell JC, Aspegrén J, McKusick BC, Hellebrekers LJ. Dexmedetomidine constant rate infusion for 24 hours during and after propofol or isoflurane anaesthesia in dogs. Randomized Controlled Trial Vet Anaesth Analg. 2008 Mar;35(2):141-53.
11
3 FDA Freedom of Information
https://animaldrugsatfda.fda.gov/adafda/app/search/public/document/downloadFoi/12187#:~:text=Zenalpha%C2%AE%20%28medetomidine% 20and%20vatinoxan%20hydrochlorides%20injection%29%20is%20approved,clinical%20examination%2C%20clinical%20procedures%20and %20minor%20surgical%20procedures
4 Ketamine: Does Life Begin at 40? IASP Pain Clinical Updates, Carr DB, ed. XV:3, June 2007
5 Slingsby LS, Waterman-Pearson AE, The postoperative analgesic effects of ketamine after canine ovariohysterectomy – a comparison between pre- and post-operative administration. Res Vet Sci. 2000 Oct;69(2):147-52
6 Boscan P, Pypendop BH, Solano AM, Ilkiw JE. Cardiovascular and respiratory effects of ketamine infusions in isoflurane-anesthetized dogs before and during noxious stimulation. Am J Vet Res. 2005 Dec;66(12):2122-9.
7 McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs. 2010 Jun 18;70(9):1149-63
8 Kranke P, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart LH, Poepping DM, Weibel S. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 2015 Jul 16;(7):CD009642.
9 Weibel S, Jelting Y, Pace NL, Helf A, Eberhart LH, Hahnenkamp K, Hollmann MW, Poepping DM, Schnabel A, Kranke P. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. Cochrane Database Syst Rev. 2018 Jun 4;6:CD009642.
10 Bailey M, Corcoran T, Schug S, Toner A. Perioperative lidocaine infusions for the prevention of chronic postsurgical pain: a systematic review and meta-analysis of efficacy and safety. Pain. 2018 May 1. doi: 10.1097/j.pain.0000000000001273. [Epub ahead of print]
11 Cahana A, Shvelzon V, et al. Intravenous lignocaine for chronic pain: an 18-month experience. Harefuah. 1998 May 1;134(9):692-4, 751, 750
12 Muir WW 3rd, Wiese AJ, March PA. Effects of morphine, lidocaine, ketamine, and morphine-lidocaine-ketamine drug combination on minimum alveolar concentration in dogs anesthetized with isoflurane. Am J Vet Res. 2003 Sep;64(9):1155-60.
13 Ochi H, Hara Y, Asou Y, Harada Y, Nezu Y, Yogo T, Shinomiya K, Tagawa M. Effects of long-term administration of carprofen on healing of a tibial osteotomy in dogs. Am J Vet Res. 2011 May;72(5):634-41.
14 Dodwell ER, Latorre JG, Parisini E, Sweltler E, Chandra D, Mulpuri K, Snyder. NSAID exposure and risk of nonunion: a meta-analysis of case-control and cohort studies. Review Calcif Tissue Int. 2010 Sep;87(3):193-202.
15 Gallaher HM, Butler JR, Wills RW, Priddy LB, Elder SH, Heller SM, Brinkman E, Baumgartner W. Effects of short- and long-term administration of nonsteroidal anti-inflammatory drugs on osteotomy healing in dogs. Vet Surg. 2019 Oct;48(7):1318-1329.
16 Rushfeldt CR, Sveinbjørnsson B, Søreide K, Vonen B. Risk of anastomotic leakage with use of NSAIDs after gastrointestinal surgery. Review Int J Colorectal Dis. 2011 Dec;26(12):1501-9.
17 Taylor PM, Luangdilok CH, Sear JW. Pharmacokinetic and pharmacodynamic evaluation of high doses of buprenorphine delivered via high-concentration formulations in cats. J Feline Med Surg. 2016 Apr;18(4):290-302
18 Watanabe R, Monteiro BP, Evangelista MC, Castonguay A, Edge D, Steagall PV. The analgesic effects of buprenorphine (Vetergesic or Simbadol) in combination with carprofen in dogs undergoing ovariohysterectomy: a randomized, blinded, clinical trial. BMC Vet Res. 2018 Oct 5;14(1):304.
19 Kinobe RT, Miyake Y. Evaluating the anti-inflammatory and analgesic properties of maropitant: A systematic review and meta-analysis. Meta-Analysis Vet J. May-Jun 2020;259-260:105471.
20 Soares PCLR, Correa JMX, Niella RV, de Oliveria JNS, Costa BA, Silva AC, Sena AS, Pinto TM, Munhoz AD, Martins LAF, Silva EB, Lavor ML. Continuous Infusion of Ketamine and Lidocaine Either with or without Maropitant as an Adjuvant Agent for Analgesia in Female Dogs Undergoing Mastectomy. Vet Med Int. 2021 Jan 26;2021:4747301
21 Hegron A, Peach CJ, Tonello R, Seemann P, Teng S, Latorre R, Huebner H, Weikert D, Rienties J, Veldhuis NA, Poole DP, Jensen DD, Thomsen ARB, Schmidt BL, Imlach WL, Gmeiner P, Bunnett NW. Therapeutic antagonism of the neurokinin 1 receptor in endosomes provides sustained pain relief. Proc Natl Acad Sci U S A. 2023 May 30;120(22):e2220979120
22 Kukanich B, Papich MG. Pharmacokinetics of tramadol and the metabolite O-desmethlytramadol in dogs, J. Vet. Pharmacol. Therap. 27, 239–246, 2004
23 McMillan CJ, Livingston A, Clark CR et al. Pharmacokinetics of intravenous tramadol in dogs. Can J Vet Res. 2008 Jul;72(4):325-31
24 Donati PA, Tarragona L, Franco JVA, Kreil V, Fravega R, Diaz A, Verdier N, Otero PE. Efficacy of tramadol for postoperative pain management in dogs: systematic review and meta-analysis. Vet Anaesth Analg. 2021 May;48(3):283-296.
25 Pypendop BH, Ilkiw JE. Pharmacokinetics of tramadol, and its metabolite O-desmethyl-tramadol, in cats. J Vet Pharmacol Ther. 2008 Feb;31(1):52-9.
26 Evangelista MC, Silva RA, Cardozo LB, Kahvegian MA, Rossetto TC, Matera JM, Fantoni DT. Comparison of preoperative tramadol and pethidine on postoperative pain in cats undergoing ovariohysterectomy. BMC Vet Res. 2014 Oct 15;10:252.
27 Longmire DR, Jay GW, Boswell MV. Neuropathic Pain. In: Weiner’s Pain Management, A Practical Guide for Clinicians, 7th ed. Boswell MV, Cole BE ed. Taylor & Francis, Boca Raton FL 2006, p. 305.
28 Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2011 Mar 16;(3)
29 Ho KY, Gan TJ, Habib AS. Gabapentin and postoperative pain a systematic review of randomized controlled trials.Pain. 2006 Dec 15;126(1-3):91-101
30 Hurley RW, Coehn SP, Williams KA, et al. The analgesic effects of perioperative gabapentin on postoperative pain: a meta-analysis. Reg Anesth Pain Med. 2006 May-Jun;31(3):237-47.
31 Tippana EM, Hamunen K, Kontinen VK, Kalso E. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg. 2007 Jun;104(6):1545-56
32 Seib RK, Paul JE. Preoperative gabapentin for postoperative analgesia: a meta-analysis. Can J Anaesth. 2006 May;53(5):461-9.
33Clivatti J, Sakata RK, Issv AM. Review of the use of gabapentin in the control of postoperative pain. Rev Bras Anestesiol. 2009 JanFeb;59(1):87-98
34Dauri M, Faria S, Gatti A, et al. Gabapentin and pregabalin for the acute post-operative pain management. A systematic-narrative review of the recent clinical evidences. Curr Drug Targets. 2009 Aug;10(8):716-33
12
35 Vollmer KO, von Hodenberg A, Kölle EU Arzneimittelforschung Pharmacokinetics and metabolism of gabapentin in rat, dog and man. 1986 May;36(5):830-9.
36 Schmidt PC, Ruchelli G, Mackey SC, Carroll IR. Perioperative gabapentinoids: choice of agent, dose, timing, and effects on chronic postsurgical pain. Anesthesiology. 2013 Nov;119(5):1215-21.
37 Sikina ER, Bach JF, Lin Z, Gehring R, KuKanich B. Bioavailability of suppository acetaminophen in healthy and hospitalized ill dogs. J Vet Pharmacol Ther. 2018 May 13. doi: 10.1111/jvp.12664. [Epub ahead of print]
38 Bello AM, Dye C. Current perceptions and use of paracetamol in dogs among veterinary surgeons working in the United Kingdom. Vet Med Sci. 2023 Mar;9(2):679-686.
39 Benitez ME, Roush JK, McMurphy R, KuKanich B, Legallet C. Clinical efficacy of hydrocodone-acetaminophen and tramadol for control of postoperative pain in dogs following tibial plateau leveling osteotomy.
40 Budsberg SC, Kleine SA, Norton MM, Sandberg GS, Papich MG. Comparison of the effects on lameness of orally administered acetaminophen-codeine and carprofen in dogs with experimentally induced synovitis. Am J Vet Res. 2020 Aug;81(8):627-634.
41Drygas KA, McClure SR, Goring L, Pozzi A, Robertson SA, Wang C. Effect of cold compression therapy on postoperative pain, swelling, range of motion, and lameness after tibial plateau leveling osteotomy in dogs. J Am Vet Med Assoc. 2011 May 15;238(10):1284-91.
42 von Freeden N,, Duerr F, Fehr M, Diekmann C, Mandel C, Harms O. Comparison of two cold compression therapy protocols after tibial plateau leveling osteotomy in dogs. Tierarztl Prax Ausg K Kleintiere Heimtiere. 2017 Aug 10;45(4):226-233.
43 Rogatko CP Baltzer WI, Tennant R. Preoperative low level laser therapy in dogs undergoing tibial plateau levelling osteotomy: A blinded, prospective, randomized clinical trial. Vet Comp Orthop Traumatol. 2017 Jan 16;30(1):46-53.
44 Renwick SM, Renwick AI, Brodbelt DC, Ferguson J, Abreu H. nfluence of class IV laser therapy on the outcomes of tibial plateau leveling osteotomy in dogs. Vet Surg..2018 May;47(4):507-515.
45 Kennedy KC, Martinez SA, Martinez SE, Tucker RL, Davies NM. Effects of low-level laser therapy on bone healing and signs of pain in dogs following tibial plateau leveling osteotomy. Am J Vet Res. 2018 Aug;79(8):893-904
13
Locoregional Anesthesia –Part 1
14
Locoregional Anesthesia – Part 1
Mark Epstein DVM, DABVP (C/F), CVPP
TotalBond Veterinary Hospitals
Gastonia & Charlotte, NC USA
International Veterinary Academy of Pain Management
Local anesthetics were once a mainstay of pain management in veterinary medicine, and may now be one of the most under-utilized modalities. There are many reasons to combine general and local anesthetic for surgical pain relief. 1 Local anesthetic drugs are extremely effective, inexpensive and easy to use. When local anesthetic drugs are administered, pain impulses originating in the periphery are blocked and prevented from reaching the central nervous system. This blockade has several positive consequences:
• The sensation of pain is alleviated or even eliminated for the duration of the block. Local anesthetic drugs work by blocking sodium channels in nerve membranes. Decreased permeability to sodium slows the rate of depolarization so that the threshold potential is not achieved and an action potential is not propagated, thus the pain impulse is not propagated. Local anesthetics bind more readily to ‘open’ channels, thus rapidly firing nerves are more susceptible to blockade.
• The likelihood that ‘wind-up’ or hypersensitization will occur in the dorsal horn of the spinal cord is greatly decreased because the portion of the pain pathway called ‘transmission’ is blocked; this results in a lower incidence of exaggerated, sustained (i.e. maladaptive, neuropathic) pain states..
• The analgesia allows the patient to be maintained under a lighter plane of anesthesia and this makes the anesthetic episode safer for the patient. In fact, local anesthetic drugs decrease the minimum alveolar concentration (MAC) of all anesthetic gases and propofol.
• Creates a sparing effect of other analgesic medications, especially opioids and their attendant adverse effects
• Local anesthetics are recognized to have many beneficial effects beyond blocking nerve conduction; broad anti-inflammatory effects (reduced production of eicosanoids, thromboxane, leukotriene, histamine, and inflammatory cytokines; and scavenging of oxygen free radicals) and even antimicrobial, antifungal and antiviral effects. 2 . 3
• A limitation of LA is their generally short-duration of activity. However, the duration of activity can reportedly be doubled with small amounts of an opioid, either morphine (0.075 mg/kg) or buprenorphine (0.003 mg/kg) 4 , 5 or alternatively dexmedetomidine (0.002 mg/kg) which provided 24 hours of analgesia in 2/3 of dogs receiving peripheral nerve blockade. 6 New in 2016: Nocita®, a liposome-encapsulate bupivacaine product that provides up to 3 days of post-operative analgesia at the application site.
Furthermore, local anesthetic blocks are extremely cost effective and can increase profits to the clinic.
15
Commonly used local anesthetic drugs in veterinary medicine include
• Lidocaine
o Onset of action: rapid (< 5 minutes), duration of action: 60-120 minutes
o Infiltrative dose 2-6 mg/kg (use the lower end of the dose in cats)
o Convulsive dose in dogs: 11-20 mg/kg
o Lethal dose in dogs: 16-28 mg/kg
o ‘Toxic dose’ in cats reported as 6-10 mg/kg
o The general recommendation for clinical use is ≤ 6 mg/kg in the dog and ≤ 3-4 mg/kg in the cat.
• Bupivacaine
o Onset of action: approximately 10 minutes after injection (up to 20 minutes), duration of action: 4 to 6 hours
o Infiltrative dose 1-2 –(4) mg/kg (use the lower end of the dose in cats)
o Toxic dose in dogs: 5-11 mg/kg or potentially any amount given IV
o Data is mostly anecdotal in the cat but the general feeling is that 3 mg/kg is the toxic dose.
o The general recommendation for clinical use is ≤ 2 mg/kg in the dog and ≤ 1 mg/kg in the cat.
• Ropivacaine
o Onset of action: 5-10min, duration of action: 4-6H
o Infiltrative dose 1-2 mg/kg (lower end of range in cats)
o Much safer cardiovascular safety than bupivacaine, but advised 3 mg/kg max
• Mepivacaine
o Onset of action like lidocaine, <5 min, duration 1-2 hours
o In awake animals does not sting as much as other LA’s
o Dose 2.5 mg/kg cats, 5.0 mg/kg cats
Adverse events caused by local anesthetic drugs: rare but can include any of the following:
• Local tissue effects – swelling, bleeding, inflammation, dysthesias (‘tingling’? unknown if this occurs in animals) A commonly held misconception is that local anesthetics impair wound healing – although they can powerfully inhibit the inflammatory component of cellular tissue influx, there is no evidence to support a clinical effect of impaired wound healing. Both bupivacaine and ropivacaine have been implicated in myotoxicity when injected IM, although this has not been listed as a complication in most human studies where these drugs were infused for 24 – 36 hours postoperatively into a wound bed. Anaphylaxis – rare, more common with esters (but still rare)
• Central nervous system – muscle tremors, seizure, coma. At lower concentrations, depression of inhibitory neurons occurs and can cause cerebral excitation, which may lead to seizures. At higher concentrations, profound CNS depression with subsequent coma, respiratory arrest and death can occur. This AE is more likely following IV boluses of large doses of lidocaine
16
• Cardiovascular system – the myocardial conduction system is sensitive to local anesthetics and IV boluses can result in cardiovascular collapse. ONLY LIDOCAINE CAN BE ADMINISTERED IV (and never with epinephrine).
• Methemoglobinemia – rare, but can occur in cats.
• Motor and autonomic nerves are also blocked by local anesthetics, and so motor weakness and vasodilation may occur with certain techniques. Blockade of essential nerve function, like that of phrenic nerve, or high epidural blocks, should be avoided. Motor weakness or paralysis of limbs, from spinal or major nerve trunk blockade is transient and as long as the patient is protected from injury and undue stress, should not be of consequence.
Liposome-Encapsulated Bupivacaine
In 2016, an extended-release, LE-bupivacaine was FDA-approved for dogs undergoing stifle surgery (Nocita™, Aratana, since purchased by Elanco), eliciting 3-days of analgesic effect; in 2018 the label was extended to nerve block for digit surgery (onychectomy) in cats. The product has been available for several years in humans under the trade name Experel™. As the liposomes degrade, bupivacaine is released into the surrounding tissue, rendering its local anesthetic effect. The product itself is viscous and does not readily diffuse, therefore the label calls for utilizing an “advancing needle” technique whereby the product is deposited by repeat injections into the affected tissue, at each layer upon closure. A number of extralabel uses have been described.
1 Jones RS. Combining local and general anesthesia for better pain relief in dogs and cats. Vet J. 2008 Nov. 178(2):161-2
2 Cassuto J, Sinclair R, Bonderovic M. Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaestheesiol Scand. 2006 Mar; 50(3): 265-8
3Johnson SM, Saint John BE, Dine AP. Local anesthetics as antimicrobial agents: a review. Surg Infect (Larchmt). 2008 Apr;9(2):205-13.
4 Candido KD, Winnie AP, Ghaleb AH, Fattouh MW, Franco CD. Buprenorphine added to the local anesthetic for axillary brachial plexus block prolongs post-operative analgesia. Reg Anesth Pain Med. 2002 Mar-Apr;27(2):162-7
5 Bazin JE, Massoni C, Bruelle P, Fenies V, Groslier D, Schoeffler P. The addition of opioids to local anesthetics in brachial plexus block: the comparative effects of morphine, buprenorphine, and sufentani. Anaesthesia. 1997 Sep;52(9):858-62
6 Bartel AK, Campoy L, Martin-Flores M, Gleed RD, Walker KJ, Scanapico CE, Reichard AB. Comparison of bupivacaine and dexmedetomidine femoral and sciatic nerve blocks with bupivacaine and buprenorphine epidural injection for stifle arthroplasty in dogs. Vet Anaesth Analg. 2016 Jul;43(4):435-43.
17
Locoregional Anesthesia –Part 2
18
Locoregional Anesthesia – Part 2
Mark Epstein DVM, DABVP (C/F), CVPP
TotalBond Veterinary Hospitals
Gastonia & Charlotte, NC USA
International Veterinary Academy of Pain Management
LOCOREGIONAL APPLICATIONS: The locality of administration is often limited only by the clinician’s ability to learn various utilities and anatomic landmarks; few are outside the scope of any clinician to master. For many of the blocks listed below, a suggested volume of drug is listed based on the amount of drug that can physically be injected into the site. However, with all blocks, the total dose that the patient can receive should be calculated and the cumulative dose (add up the dose or volume injected for each block) should not exceed this total dose.
1. Transdermal/cutaneous
a. Commercial transdermal products are extremely useful in facilitating catheter placement and for minor procedures involving the dermis and epidermis. A lidocaine/prilocaine ointment formulation (EMLA®, also comes as a generic) is placed on a shaved area and covered with a non-porous wrap (foil or cellophane). In humans it is recommended to have the product in place for 45 minutes to achieve full affect, but in the author’s experience 15-20 minutes appears sufficient in dogs and cats. Penetration depth of analgesia has been reported to be time dependent and from 2-6 mm. 1
b. Commercial 5% lidocaine patches (Lidoderm®) provides post-operative wound paraincisional analgesia. 2 However, Lidoderm® patches in fact are manufactured and labeled for post-herpetic neuralgia (Shingles), a very common form of chronic, neuropathic pain in humans. The pharmacokinetics of this product has been investigated in dogs and cats, with minimal systemic absorption noted. 3 , 4 The adhesive patches can be cut formed to the desired size and shape, for example on either side of an incision. One cautionary note is that an entire patch contains 700 mg of lidocaine, obviously a dose that would be toxic if ingested; therefore, adequate precautions need to be taken to ensure the patient is unable to access the patch. A recent study with Lidoderm® patches in dogs undergoing ovariohysterectomy failed to demonstrated additional incisional pain relief vs. the control group. 5 This suggests the greater utility may be in hyperalgesic (i.e. hypersensitized) than for routine post-surgical pain, but more studies are necessary.
c. Studies in humans with moderate-severe stifle osteoarthritis reveal significant reduction in pain intensity after 2-week use of Lidoderm® patches 6, and pain relief similar to that achieved by oral NSAID. 7 Their potential for use in animals for chronic pain conditions (e.g. osteoarthritis, osteomyelitis, osteosarcoma) remains plausible but no applications are described in the veterinary literature.
19
2. ‘Field’ block
a. Blocking the ‘field’ of surgery. Local anesthetic drugs can be administered around the incision or directly into the incision. It is not true that lidocaine in an incision causes a delay in healing.
b. Several veterinary studies demonstrate clinical efficacy of incisional local anesthetic. 8 , 9 Two studies were unable to discern a difference using incisional LA; however these results may have been confounded by low dose, 10 technique errors and use of other analgesic medications. 11 Fitzpatrick et al (2010) In humans the overall preponderance of data including several systematic reviews supports the ability of incisional blocks to improve a number of outcome measures including patient comfort, reduction in use of opioids, earlier discharge, and diminished chronic pain states.
3. Intra-cavitary
a. Intraperitoneal bupivacaine (at a relatively high dose, 4.4 mg/kg) has demonstrated safety and a positive effect in dogs 12 , 13 , 14 and cats 15 , 16 undergoing ovariohysterectomy, but can be surmised to have benefit in any laparotomy procedure. This is supported by multiple studies of similar techniques in humans having laparotomy. In humans intra-peritoneal (and even intra-pleural) infusions of bupivacaine are used to alleviate pain from pancreatitis. 17
b. The bupivacaine (2 mg/kg) may be squired directly in to the abdominal cavity or diluted in saline and left in as a final abdominal lavage. In a closed cavity (chest 18 or abdomen), the bupivacaine can be injected through a catheter.
Oral blocks: Blocks listed below will cause unilateral desensitization from the site of injection rostrally to midline.
4. Maxillary or infraorbital nerve block
a. cranial approach
i. The infraorbital nerve exits the infraorbital foramen, which can be palpated as a depression in the buccal mucosa dorsal to the distal root of the maxillary 3rd premolar (just cranial to the root of the 4th premolar or carnassial tooth in the area where the gingiva on the maxillary bone and the gingiva on the lip join together).
ii. Block the nerve by injecting local anesthetic under the gingiva just rostral to the foramen or insert the tip of the needle into the infraorbital canal and inject. Injecting into the foramen insures more caudal spread of the block but is not necessary if the oral surgery site is rostral to the foramen Also, the foramen can be difficult to locate or to enter in small dogs and cats & infusion rostral to the canal is still useful as there will be some caudal migration of the local anesthetic into the canal.
iii. A vessel runs with this nerve so aspirate, then slowly infuse drug (0.1 to 1.0 ml).
20
b. caudal approach – will also block molars and caudal carnassial
i. Insert the needle percutaneously along the ventral border of the zygomatic process approximately 0.5 cm caudal to the lateral canthus of the eye. The needle is directed medially and slightly cranially (in an angle that would draw an imaginary line with the premolars on the opposite side of the head) until it hits bone. At this site, the maxillary nerve enters the pterygopalatine fossa. Aspirate and slowly inject 0.1-1.0 mls local anesthetic.
ii. An alternate technique is to approach the pterygopalatine fossa from the ventral margin of the orbit.
5. Mandibular nerve block
i. The mandibular foramen or the mandibular nerve can often be palpated on the lingual side of the mandible just rostral to the angle of the mandible and just caudal to the last molar in approximately the middle 1/3rd of the mandible (as measured from top to bottom).
ii. Regardless of whether or not the nerve or foramen can be palpated (often difficult to palpate in very small patients), the landmarks described above will be utilized for deposition of local anesthetic drug.
iii. The nerve ENTERS the mandible at the mandibular foramen and cannot be blocked between the mandibular foramen and the mental foramen. Extraoral technique: approach is from the outside, through the skin at the angle of the mandible. This technique is easier than the intraoral technique in cats and in some small dogs.
1. Pass the needle through the skin along the medial aspect of the mandible with the needle perpendicular to the mandibular cortical bone, to the level of the foramen (again, aiming for a site just caudal to the last molar on the lingual side of the mandible).
2. With a finger in the oral cavity the needle can be felt under the gingiva.
3. When the site near the mandibular foramen is reached, aspirate and inject the local anesthetic drug (0.2-2.0 mls).
6. Testicular block
a. Data for benefit in both dogs 19 , 20 and cats 21 , 22
b. Isolate body of testicles; insert needle to cranial pole and give extended aspiration to make sure not in vessel. Inject lidocaine or bupivacaine into the body of the testicle until you feel ‘pressure’.
i. Drug will migrate up spermatic cord; takes approx. 10-15 min for max. effect.
c. Generally, ½-2 ml per testicle in cats/small dogs and larger dogs, respectively
d. For incision directly over testicle, continue infiltrating as the needle exits the testicular body to block the skin and subcutaneous tissue; don’t forget to block prescrotal incision site if used!
21
7. Mesovarium block
a. Data mixed: effective in cat 23 but not demonstrated in dog 24
b. Isolate each pedicle and with 25g needle, aspirate and inject small volume (0.1-0.2 ml) of lidocaine into mesovarium
c. Some also advocate injecting into uterine body
8. Digit or paw block
a. Cats via four-point point) 25 Enomoto
i. Locate the carpus and the accessory carpal pad and inject 0.1-0.3 mls subcutaneously at three sites:
1. medial to the accessory carpal pad (blocks median nerve and palmar branch of the ulnar nerve);
2. lateral and proximal to the accessory carpal pad (blocks dorsal branch of the ulnar nerve); and
3. on the dorsal-medial portion of the carpus (blocks superficial branches of the radial nerve).
b. Single Digit Ring block
i. Deploy a subcutaneous ‘line’ of local anesthetic circumferentially all the way around P1 of target digit
c. IV Regional Anesthesia (IVRA, “Bier block”) 26
i. Blood exsanguinated from cephalic vein by distal proximal occlusion
ii. Tourniquet is placed on cephalic vein firm enough to occlude venous but not arterial flow
iii. Lidocaine 2 mg/kg (no epi!) is injected IV (some use catheter, some not); has been demonstrated safe in cats as well. 27
iv. Will take approx. 10-15 min for full effect, will block distal limb; max time for tourniquet 90 min.; do not remove tourniquet any earlier than 20 min. post injection to avoid IV bolus.
9. Intercostal block 28
a. Indicated for rib fractures, chest tubes, thoracotomy
b. With needle directed perpendicularly to skin, inject local anesthetic in the tissues caudal to the proximal portion of the ribs (the adjacent artery and vein are actually underneath this aspect of the rib). Inject local anesthetic in 2-3 rib spaces in front of and 2-3 rib spaces behind the area that needs to be desensitized.
10. Sacro-coccygeal block 29
a. Indicated for perineal, tail procedures including: relief of urinary obstruction, perineal urethrostomy, anal sacculectomy, peri-anal mass removal, tail amputation
b. Patient is placed in sternal recumbency, palpate the space between the sacrum and the 1st coccygeal vertebra while dorsiflexing tail (between Cx 1-2 also acceptable)
c. Clip & prep, Use a 25ga 1” needle to penetrate the skin at midline
22
d. Direct the needle at a 30 to 45-degree angle and continue through the inter arcuate ligament
e. There may be a palpable “pop” when the ligament is penetrated; as the needle is advanced, there is no resistance upon entering the epidural space
f. If bone is encountered, keep the needle in the skin and slightly angle the needle cranially or caudally off the bone until the space is entered
g. The needle feels more firmly seated once the ligament is penetrated than it does in the subcutaneous tissues
h. Inject 0.5 ml of 2% lidocaine or 0.5% bupivacaine; there should be no resistance
11. Intra-articular block
a. This block is used for analgesia pre- and post-closure for intraarticular surgery. Inject 1-5 ml local anesthetic into the joint prior to surgery and repeat the injection after the joint has been sutured closed.
b. In vitro studies have demonstrated chondrotoxicity of 0.5% bupivacaine and 2% lidocaine; 30 the clinical significance of single application is uncertain as residence time in the canine arthritic joint is relatively short (30-60 min) 31
c. If local anesthetics are concerning, use opioids! There are opioid receptors in the synovium and they are upregulated in inflammation.
d. The techniques are also suitable for IA injection of biologic agents e.g. Plateletrich plasma, stem cells etc.
12. Retrobulbar block 32 , 33
a. 22 g 1 1/2” needle in most cases, some prefer with a sterile gloved-hand to place a 10-degree bend in the middle.
b. Palpate the dorsal edge of the lateral aspect of the zygomatic arch; penetrate the skin with the needle roughly horizontal to the muzzle
c. Advance the needle caudo-medially to come up underneath the globe, then angle dorsally to come up into the space behind the globe. Aspirate and inject
d. This block does not affect the lids; if performed for enucleation then infiltration of LA into the lid margins should occur before excision; some advocate splash block into the globe as well.
13. Regional nerve block techniques (generally performed with electro- or ultrasound location devices) 34: The reader is directed to a comprehensive resource:
• Portela et al, Regional anesthetic techniques for the thoracic limb and thorax in small animals: A review of the literature and technique description. Vet J. 2018 Nov;241:8-19.
• Portela et al, Regional anesthetic techniques for the pelvic limb and abdominal wall in small animals: A review of the literature and technique description. Vet J. 2018 Aug;238:27-40.
• Read M, Campoy L. Small Animal Regional Anesthesia and Analgesia 1st Ed. Wiley-Blackwell, Ames, IA 2013.
a. Brachial Plexus
b. Radial, Ulnar, Median/Musculocutaneous
c. Femoral nerve
d. Sciatic nerve
23
References for technique descriptions:
Skarda, RT, Local and regional anesthetic and analgesic techniques: dogs. In: Lumb and Jones’ Veterinary Anesthesia, Third Ed., Thurmon, Tranquilli, & Benson, eds., Williams and Wilkins, p 426-447, 1996.
Tranquilli WJ, Grimm, KA, Lamont LA. Pain Management for the Small Animal Practitioner Teton New Media Jackson, WY, 2000.
1 Wahlgren CF, Quiding H. Depth of cutaneous analgesia after application of a eutectic mixture of the local anesthetics lidocaine and prilocaine (EMLA cream). J Am Acad Dermatol. 2000 Apr;42(4):584-8
2 Weil AB, Ko J, Inoue T. The use of lidocaine patches. Comp Cont Ed April 2007 29(4):208-16
3 Weiland L, Croubels S, Baert K, Polis I, De Backer P, Gasthuys Fl. Pharmacokinetics of a lidocaine patch 5% in dogs. J Vet Med A Physiol Pathol Clin Med. 2006 Feb;53(1):34-9
4 Ko JC, Maxwell LK, Abbo LA, Weil AB. Pharmacokinetics of lidocaine following the application of 5% lidocaine patches to cats. J Vet Pharmacol Ther. 2008 Aug;31(4):359-67.
5 Merema DK, Schoenrock EK, Le Boedec K, McMichael MA. Effects of a transdermal lidocaine patch on indicators of postoperative pain in dogs undergoing midline ovariohysterectomy. J Am Vet Med Assoc. 2017 May 15;250(10):1140-1147.
6 Galer BS, Sheldon E, et al, topical lidocaine patch 5% may target a novel underlying pain mechanism in osteoarthritis. Curr med Res Opin 20(9):1455-1458, 2004
7 Kivitz A, Fairfax M. Sheldon EA, Xiang Q, Jones BA, Gammaitoni AR, Gould EM. Comparison of the effectiveness and tolerability of lidocaine patch 5% versus celecoxib for osteoarthritis-related knee pain: post hoc analysis of a 12 week, prospective, randomized, active-controlled, open-label, parallel-group trial in adults. Clin Ther. 2008 Dec;30(12):2366-77
8 Savvas I, Papzoglous LG, Kazakos G, Anagnostou T, Tsioli V, Raptapoulos De. Incisional block with bupivacaine for analgesia after celiotomy in dogs. J Am Anim Hosp Assoc. 2008 Mar-Apr;44(2):60-6.
9 Carpenter RE, Wilson DV, Evans AT. Evaluation of intraperitoneal and incisional lidocaine or bupivacaine for analgesia following ovariohysterectomy in the dog. Vet Anaesth Analg. 2004 Jan;31(1):46-52.
10 Tobias KM, Harvey RC, Byarlay JM. A comparison of four methods of analgesia in cats following ovariohysterectomy. Vet Anaesth Analg. 2006 Nov;33(6):390-8.
11 Fitzpatrick CL, Weir HL, Monnet E. Effects of infiltration of the incision site with bupivacaine on post-operative pain and incisional healing in dogs undergoing OHE. 2010 J Am Vet Med Assoc. 237:4
12 Carpenter RE, Wilson DV, Evans AT. Evaluation of intraperitoneal and incisional lidocaine or bupivacaine for analgesia following ovariohysterectomy in the dog. Vet Anaesth Analg. 2004 Jan;31(1):46-52.
13 Wilson DV, Barnes KS, Hauptman JG. Pharmacokinetics of combined intraperitoneal and incisional lidocaine in the dog following ovariohysterectomy. J Vet Pharmacol Ther. 2004 Apr;27(2):105-9
14 Campagnol D, Teixeira-Neto FJ, Monteiro ER, Restitutti F, Minto BW., Effect of intraperitoneal or incisional bupivacaine on pain and the analgesic requirement after ovariohysterectomy in dogs.
15 Benito J, Monteiro BP, Beaudry F, Lavoie AM, Lascelles BD, Steagall PV. Pharmacokinetics of bupivacaine after intraperitoneal administration to cats undergoing ovariohysterectomy. Am J Vet Res. 2016 Jun;77(6):641-5.
16 Benito J, Monteiro B, Lavoie AM, Beauchamp G, Lascelles BDX, Steagall PV. Analgesic efficacy of intraperitoneal administration of bupivacaine in cats. J Feline Med Surg. 2016 Nov;18(11):906-912.
17 Dravid RM, Paul RE. Interpleural block - part 2. Anaesthesia. 2007 Nov;62(11):1143-53.
18 Conzemius MG, Brockman DJ, King LG, Perkowski SZ. Analgesia in dogs after intercostal thoracotomy: a clinical trial comparing intravenous buprenorphine and interpleural bupivacaine. Vet Surg. 1994 Jul-Aug;23(4):291-8.
19 McMillan MW, Seymour CJ, Brearley JC. Effect of intratesticular lidocaine on isoflurane requirements in dogs undergoing routine castration. J Small Anim Pract. 2012 Jul;53(7):393-7.
20 Huuskonen V, Hughes JL, Estaca Bañon E, West E. Intratesticular lidocaine reduces the response to surgical castration in dogs. Vet Anaesth Analg. 2013 Jan;40(1):74-82.
21 Moldal ER, Kirpensteijn J, Kristensen AT, Haga HA, Nødtvedt A, Eriksen T. Evaluation of inflammatory and hemostatic surgical stress responses in male cats after castration under general anesthesia with or without local anesthesia. Am J Vet Res. 2012 Nov;73(11):1824-31.
22 Moldal ER, Eriksen T, Kirpensteijn J, Nødtvedt A, Kristensen AT, Sparta FM, Haga HA. Intratesticular and subcutaneous lidocaine alters the intraoperative haemodynamic responses and heart rate variability in male cat Bubalo V, Moens YP, Holzmann A, Coppens P. Anaesthetic sparing effect of local anaesthesia of the ovarian pedicle during ovariohysterectomy in dogs. Vet Anaesth Analg. 2008 Nov;35(6):537-42. s undergoing castration. Vet Anaesth Analg. 2013 Jan;40(1):63-73.
23 Zilbersetin LF, Moens YP, Leterrier E. The effect of local anaesthesia on anaesthetic requirements for feline ovariectomy. The Vet J 2008;178: 212–216.
24
25 Curcio K, Bidwell LA, Bohart GV, Hauptman JG. Evaluation of signs of postoperative pain and complications after forelimb onychectomy in cats receiving buprenorphine alone or with bupivacaine administered as a four-point regional nerve block. J Am Vet Med Assoc. 2006 Jan 1;228(1):65-8.
26 Webb AA, Cantwell SL, Duke T, Adkins E. Intravenous regional anesthesia (Bier block) in a dog. Can Vet J. 1999 June: 40(6):419-21
27 Kushner LI, Fan B, Shofer FS. Intravenous Regional Anesthesia in Isoflurane Anesthetized Cats: Lidocaine Plasma Concentrations and Cardiovascular Effects. Vet Anaesth Analg. July 2002;29(3):140-149. 32
28 Pascoe PJ, Dyson DH. Analgesia after lateral thoractoomy in dogs. Epidural morphine vs. intercostal bupivacaine. Vet Surg. 1993 Mar-Apr;22(2):141-7.
29 O’Heran AK, et al. Coccygeal epidural with local anesthetic for catheterization and pain management in the treatment of feline urethral obstruction. J Vet Emerg Crit Care 2011;21(1):50-52.
30 Chu CR, et al. The in vitro effects of bupivacaine on articular chondrocytes. J Bone Joint Surg Br. 2008 Jun;90(6):814-20.
31 Barry SL, Martinez SA, Davies NM, Bachelez A, Remsberg CM, Liu M. Synovial Fluid Concentrations of Bupivacaine Following Single Intra-Articular Injection in Canine Osteoarthritic Stifles. ACVS Proceedings 2011
32 Accola et al, Development of a retrobulbar injection technique for ocular surgery and analgesia in dogs. JAVMA July 15, 2006, Vol. 229, No. 2, Pages 220-225
33 Myrna KE, et al. Effectiveness of injection of local anesthetic into the retrobulbar space for postoperative analgesia following eye enucleation in dogs. J Am Vet Med Assoc. 2010 237:2, 174-177
34 Campoy L & Read M (Editors): Small Animal Regional Anesthesia and Analgesia 1st Edition, Wiley-Blackwell, Ames IA 2013
25
Oral Medications for the Chronic Pain Management
26
Oral Medications for the Chronic Pain Management
Mark Epstein DVM, DABVP (C/F), CVPP
TotalBond Veterinary Hospitals
Gastonia & Charlotte, NC USA
International Veterinary Academy of Pain Management
Introduction
Outside the realm of NSAID and opioid exist a broad range of medications that exert an analgesic effect, or otherwise modify and protect against pain, by manipulating various targets along the nociceptive pathway. This session will focus on those medications administered by the oral route.
TRAMADOL
In humans, tramadol is known to exert its pain-modifying effect through two metabolites; one enhances inhibitory neurotransmitters (serotonin, norepinephrine), and the other (0-desmethyltramadol, “ODM” or “M1”) metabolite is a weak opioid (1/100th the mu-receptor affinity of morphine. However, in contradistinction to humans, tramadol has a very short half-life (1.1 – 1.5 hours) in the dog 1 (humans: 5-6 hours for parent compound and metabolites), and it appears that dogs produce negligible amounts of M1 opioid metabolite 2 ,
,
and furthermore the T1/2 of whatever it does produce is also very short (2.2 H) in this species. Pharmacodynamic studies in dogs have demonstrated the anesthetic-sparing 8 , 9 and painmodifying effect of parenteral tramadol 10 , 11 , 12 , 13 , 14 , 15 (presumably through serotoninergic, noradrenergic pathways, not opioid), but convincing evidence for a pain-modifying effect of oral tramadol remains is elusive at this time. 16 Worsening the PK picture in dogs: studies reveal that not only are plasma levels much lower following oral administration than in humans, sequential dosing for several days leads to dramatic reductions of those plasma levels 17 , 18 (suggesting saturation of GI active transport sites, increased metabolism, more robust first-pass effect, or a combination). One small study (6 greyhounds) of oral tramadol did report a statistically significant increase of mechanical threshold levels, but only at the 5- and 6- hour time point, 19 and using higher-than-customary doses (10 mg/kg). One study did find oral tramadol useful as part of a multi-modal analgesic protocol to control cancer pain, 20 but the specific role of tramadol is unknown and other studies have found it (not unsurprisingly) inferior as a solo agent to multi-modal analgesic approaches to control post-operative pain. 21 , 22 The short half-life of the drug suggests up to a Q-6 hour treatment regime, but there is one unpublished abstract on the effectiveness of tramadol administered once daily in canine osteoarthritis. 23 In contradistinction to dogs, cats do produce the mu-agonist M1 metabolite, 24 and a pain-modifying effect has been demonstrated in a both a thermal threshold 25 and clinical surgical model, 26 as well as a case series of use of oral tramadol in a flavored compounded form 27 (the drug is otherwise quite bitter). Toxicity, safety, and dose titration data are lacking in both dogs and cats. ADE’s encountered in humans with tramadol include gastrointestinal signs, cognitive change, agitation, hypertension, seizure potentiation, exacerbated bleeding from GI ulcers, and some concern about the potentiation of NSAID when combined with tramadol. A 2018 randomized placebo-controlled blinded study revealed that tramadol did not improve patients with canine OA. 28
3
4
5
6
7
27
,
,
,
A very recent Systematic Review and Meta-analysis revealed that the Certainty of Evidence for tramadol’s efficacy for post-surgical pain in dogs is low or very low. 29
Tapentadol (Nucytna®) is a tramadol-like drug which requires no metabolism for its opioid effect, that is, the mu agonist is the parent molecule rather than the M1 (or any other) metabolite. This feature may make it an attractive drug for dogs, however an FDA report reveals that tapentadol appears to have much lower oral bioavailability in dogs than in humans (3% vs. 32%, respectively), 30 and an equivalent regulatory report from Australia revealed minimal effect on a tail-flick assay. 31 A recent peer-reviewed study confirmed in dogs the low oral bioavailability, as well as a short plasma half-life when administered IV, but did not evaluate pharmacodynamics. 32 One other unpublished study however, did reveal a dosedependent response to IV administration of tapentadol in dogs with the tail-flick assay, similar to morphine (the tail-flick assay responds to opioids and alpha-2 agonists, not other mechanisms of antinociception such as inhibition of serotonin and/or norepinephrine), implying tapentadol does have a muagonist effect. 33 In cats, one study revealed high (>90%) bioavailability of tapentadol when delivered parenteral routes, and a T1/2 of 2-3H 34. More studies are needed to evaluate the PK, PD, and clinical utility of tapentadol in dogs and cats especially via the oral route.
GABAPENTINOIDS
Gabapentin is an anti-convulsant that analgesic properties predominantly by down-regulating presynaptic voltage-dependent calcium channels in the dorsal horn of the spinal cord 35 but other mechanisms probably exist as well (while structurally similar to GABA, it is not a direct agonist, although it may have indirect effects on GABA metabolism such as increasing intracellular stores). Because of its effectiveness and tolerability, it is approved for post-herpetic neuralgia and is in widespread use for humans with a variety of neuropathic and other maladaptive pain conditions, 36 , 37 , 38 , 39 , 40 and this suggests, along with published veterinary case reports, 41 , 42 , 43 a strong rationale for the utilization of gabapentin in analogous conditions experienced by dogs and cats. The utility of gabapentin for osteoarthritis in demonstrable in rodent models, 44 , 45 one canine study suggests a disease-modifying effect (not a pain study) in experimental osteoarthritis, 46 but no clinical studies have been published investigating gabapentin canine OA. However, case reports exist of successful use in treating non-OA neuropathic pain conditions in both dogs 47 , 48 , 49 , 50 and cats. 51 In cats, one unpublished study is reported to demonstrate a benefit of gabapentin in naturally-occurring osteoarthritis, 52 in addition to a case series of chronic musculoskeletal pain. 53
Systematic reviews in humans support safety and benefit of transoperative oral gabapentin for postsurgical pain. 54 , 55 , 56 , 57 , 58 , 59 Convincing evidence in dogs and cats for efficacy in acute pain currently is disappointing; 60 , 61 , 62 , 63 however, these studies may have been limited by under-dosing, and indeed some secondary outcome measures trending to improvement in the dogs receiving gabapentin (Aghighi 2012, trend toward lower median pain scores; Crociolli 2015 decrease opioid rescue 64). One case series utilizes gabapentin in cats with acute traumatic musculoskeletal injuries. 65
Pharmacokinetics of gabapentin are well established in dogs 66 , 67 , 68 and cats, 69 with a half-life suggesting TID administration schedule, although anecdotally BID appears to be useful.
28
The primary adverse effect in dogs appears to be somnolescence (as in humans) which usually will spontaneously resolve over a few days’ acclimation time. For chronic pain dosing, a general consensus is that doses are initiated at 3-5 mg/kg and gradually tapered upwards as the patient can tolerate to a target dose range of 20+ mg/kg. In the perioperative setting, dose based on the experience in humans is 10-15 mg/kg pre-operatively and 7-10 mg/kg B-TID post-operatively. 70 Patient populations speculated to benefit most from peri-operative gabapentin would be those suspected to have, or be at risk for, sensitization and a maladaptive pain component (e.g. severe trauma, nerve injury, pre-existing chronic inflammation).
Pregabalin is a gabapentin-like analogue and is thought to have a similar mechanism of action for both its pain-modifying (the labeled indication) and anticonvulsant (down-regulates calcium channels, diminishing action potential propagation) activity. In the U.S. it is available as Lyrica® labeled in humans for pain associated with diabetic neuropathy, fibromyalgia, and post-herpetic neuralgia (Shingles) and is a scheduled Class IV drug. It appears to have a superior kinetic profile relative to gabapentin: higher oral bioavailability, longer T ½, and with a linear GI absorption profile suggesting a dose of 4 mg/kg twice daily in the dog. 71 A case series describes its use in canine syringomyelia, 72 but its expense may currently limit its use in veterinary medicine.
AMANTADINE
Amantadine exerts a pain-modifying effect as an NMDA receptor antagonist 73 and remains an interest in humans with chronic and neuropathic pain (but not specifically osteoarthritis) in humans, with mixed results. 74 , 75 One study at 3 mg/kg once daily does demonstrate utility as an adjunct to NSAID in dogs with refractory osteoarthritis within 3 weeks, 76 and there is one case report of using amantadine to treat neuropathic pain in a dog. 77 More recent pharmacokinetic studies suggest that 3-5 mg/kg every 12 hours may be more appropriate. 78 Toxicity and kinetic studies have been performed in humans 79 and cats 80 but not in dogs. In dogs, anecdotal reports of amantadine-induced ADE’s include agitation and other behavioral changes, and GI signs especially diarrhea. In humans QT-syndrome is reported, and in dogs a recent study demonstrated a moderate risk of arrhythmia and decreased cardiac output in halothaneanesthetized dogs receiving IV amantadine. 81 The clinical significance of this finding in awake dogs receiving PO amantadine remains unknown.
TRICYCLIC ANTI-DEPRESSANTS
TCA’s exert their analgesic activity by enhancing synaptic norepinephrine and serotonin (inhibitory transmitters) in the dorsal horn of the spinal cord, although it has other effects including anti-histamine, anti-cholinergic, NMDA receptor antagonism, and sodium channel blockade. It has a balanced NE and serotonin effect, and thus is among the more sedating, anti-cholinergic, and effective of various TCA’s. 82 As a class, TCA’s are the most effective medications for neuropathic pain in humans. 83 However in dogs there exists only a single case report of utilizing amitriptyline for neuropathic musculoskeletal pain, 84 and in cats the experience in idiopathic cystitis 85 (also now termed “Pandora Syndrome” for its description as a somatic pain syndrome). In human’s TCA’s can have an unfavorable side effect profile which limit their use for neuropathic pain despite their efficacy (dry mouth, sedation, PU/PD, urine retention, blurred vision, hypotension, weight gain, agitation, seizures, cardiac arrhythmia, BM dyscrasia).
29
Customary doses of amitriptyline are 1-2 mg/kg BID in the cat and dog, but a recent review article suggests 3-4 mg/kg based on its PK profile in these species. 86
SS(N)RI’s
These compounds exert their effect by increasing serotonin +/- norepinephrine in the synaptic cleft. At least one popular SSNRI, duloxetine, has a chronic pain label in humans (including osteoarthritis and low back pain, in addition to fibromyalgia and diabetic neuropathy); one evaluation in dogs revealed poor bioavailability (4%), 87 but another study appears to reveal a dose-dependent effect with more favorable plasma levels at high doses (30 & 60 mg to laboratory beagles, equivalent to 100 & 200 mg in humans respectively which 2-4x customary dosing), but with a much shorter plasma T1/2 (2.5 H in dogs, vs. 10-12 H in humans). 88 Another SSNRI, venlafaxine (which has evidence for efficacy in human OA 89), is reported to have bioavailability approaching 50% of that of humans and T ½ of 3 hours with a suggested dose of 4 mg/kg PO Q 8-12H. 90 Evidence of a clinical pain-modifying effect for either molecule is currently lacking in animals, and there are no dosed-titration data for either drug.
Note: many drugs and compounds enhance monoamines and/or serotonin and caution should be undertaken when or if used in combination. Examples include: tramadol, TCA’s including amitriptyline and clomipramine, SS(N)RI’s, amantadine, metoclopramide, selegiline, amitraz, mirtazapine.
Trazodone is an SARI, Serotonin-antagonistic, reuptake inhibitor known for his tranquilizing, sedating, sleep-aid properties. Its reputation for modifying pain is less well established, although there are case reports for use in chronic pain and Neuropathic Itch. 91
Clonidine is an oral alpha2 agonist albeit with a resulting vasodilation rather than vasoconstriction as with parenteral dexmedetomidine. Through stimulation of pre-synaptic α2-receptors in the vasomotor center of the brainstem, presynaptic calcium levels are decreased, thus inhibiting the release of norepinephrine (NE). The net effect is a decrease in sympathetic tone, cardiac output and peripheral vascular resistance, lowering blood pressure. Therefore a primary indication in humans is for primary hypertension, and also used as an anti-anxiety, sedating, sleep-aid agent. There is anecdotal experience utilizing clonidine in humans with Neuropathic Pain. 92
Grapiprant: The first canine EP4 PRA
Grapiprant is an EP4 PRA that has demonstrated selective blockade of the EP4 receptor in rodents, humans, and dogs. Grapiprant has undergone numerous experimental and pilot studies in laboratory and client-owned dogs, and a large, multi-site, masked, placebo controlled, randomized field trial for the control of pain and inflammation associated with OA in dogs was recently completed and submitted to the FDA in support of regulatory approval. The results of these studies in client-owned dogs demonstrates that this drug at a dose of 2mg/kg/day provides control of the pain and inflammation associated with OA. Studies are currently underway investigating grapiprant in cats, and at this time data are not yet available.
As part of development of grapiprant for FDA approval for dogs with OA, a safety study in healthy Beagles investigated the effects of daily orally administered doses up to 50 mg/kg/day oral suspension (equivalent to 30.5 mg/kg/day of the tablet formulation) for nine consecutive months. There were no drug-related effects on liver enzyme values, BUN/creatinine, or platelet function. Mild and reversible dose- and timedependent decreases in total protein, albumin and calcium were seen.
30
Clinical signs were also dose dependent and restricted to mild gastrointestinal signs including soft stool, occasional stool with mucus or blood, and sporadic vomiting. There were no histopathological changes to the stomach, kidneys or liver. One dog in the 50 mg/kg group had mild mucosal regeneration of the ileum seen on histopathology.
The relative lack of toxic effects with grapiprant compared to those that have been reported in dogs treated with COX-inhibiting NSAIDs is not surprising. Grapiprant is a targeted approach to pain management it selectively blocks the EP4 receptor, does not interfere with the production of prostanoids, and therefore will not affect the other PG receptor pathways that are affected in animals treated with COX inhibitor drugs.
Galliprant® was approved in the U.S. for canine osteoarthritis in 2017; anecdotally, safety appears to very good as predicted by the safety/toxicity and pivotal trials. Pharmacokinetic and safety data has been reported in cats 93 , 94 and efficacy in rodent models of acute inflammatory pain. 95 Evidence for efficacy in dogs for acute inflammatory pain is mixed. 96 , 97
ACETAMINOPHEN (APAP, Paracetamol)
The analgesic (and anti-pyretic) mechanism of APAP in humans appears to involve inhibiting a variant COX1b (also referred to as COX3) expressing only centrally, i.e. in the brain; there appears to be no effect on peripheral COX1- or COX2-mediated inhibition of prostanoids production. A cannabinoid effect of acetaminophen is also hypothesized. Dogs do express COX1b 98, and, several older studies (not utilizing validated canine acute pain scales) reveal a pain-modifying effect in orthopedic surgery, 99 , 100 and pharmacokinetic data has been reported. 101 , 102 , 103 However, a more recent study reveals a disappointingly short (1 hour) plasma half-life and no effect on mechanical threshold in a small group of greyhound dogs, 104 and another recent PK study revealed that oral and suppository acetaminophen in healthy and clinical dogs did not reach or sustain concentrations associated with efficacy. 105 In contradistinction to humans, the literature does not appear to support that the dog has any special proclivity towards APAP-induced hepatotoxicity. This appears to be because the dog does not make the metabolite responsible for hepatotoxicity in humans (N-acetyl-p-benzoquinoneimine (NAPQI), but rather para-aminophenol (PAP) 106 , 107 which creates hematologic effects as found with cats (but without the glucoronidation problems and thus severity as found in that species). Adverse effect in dogs reported in the literature reflect (not necessarily fatal) methemoglobinemia, hemolysis, and anemia with acute overdosage 108 , 109 , 110 and in 1 case of chronic use. 111 There are no dose-titration data in dogs but a customary dose is 10-15 mg/kg PO B-TID; judicious use may or may not be appropriate in dogs. Acetaminophen is contraindicated in cats.
Naltrexone is a mu-antagonist opioid labeled to treat alcohol abuse disorder, and is also used in humans (and dogs) to treat Obsessive-Compulsive behavior disorder. However, at lower doses it appears to have analgesic and possible anti-tumor activity. 112 The former mechanism of action is postulated to be that the Levo-Naltrexone enantiomer elicits enough antagonism of mu receptors to elicit rebound production of endogenous opioids (endorphin, enkephalin). The latter is postulated to be that the Dextro-Naltrexone enantiomer antagonizes neuroinflammatory cytokines which reduces inflammation and may downregulating oncogenes.
31
The doses used in humans to achieve these effects range from only 1.0 – 4.5mg orally once daily (requires compounding as the smallest commercially available tablet size is 25mg). Extrapolating from a 180 lb person, this would translate to 0.01 – 0.05 mg/kg, with the dose for a 70-lb dog 0.3 – 1.5 mg. Naltrexone in larger doses of 50-300mg seems to negate the immunomodulatory effect by overwhelming receptors. There is 1 study in dogs with mammary carcinoma that showed higher serum concentrations of betaendorphin and met-enkephalin, fewer chemotherapy-related side effects, and better quality of life and survival rates (prolonging survival times) in the LDN-treated groups. 113
1 Kukanich B, Papich MG. Pharmacokinetics of tramadol and the metabolite O-desmethlytramadol in dogs, J. Vet. Pharmacol. Therap. 27, 239–246, 2004
2 McMillan CJ, Livingston A, Clark CR et al. Pharmacokinetics of intravenous tramadol in dogs. Can J Vet Res. 2008 Jul;72(4):325-31
3 Giorgi M, Saccomanni G, Lebkowska-Wieruszewska B, Kowalski C. Pharmacokinetic evaluation of tramadol and its major metabolites after single oral sustained tablet administration in the dog: a pilot study. Vet J. 2009 May;180(2):253-5.
4 Kukanich B, Papich MG. Pharmacokinetics and antinociceptive effects of oral tramadol hydrochloride administration in Greyhounds. Am J Vet Res 2011 Feb;72(2):256-62
5 Kögel B, Terlinden R, Schneider J. Characterisation of tramadol, morphine and tapentadol in an acute pain model in Beagle dogs. Vet Anaesth Analg. 2014 May;41(3):297-304.
6 Giorgi M, Del Carlo S, Saccomanni G, Łebkowska-Wieruszewska B, Kowalski CJ. Pharmacokinetics of tramadol and its major metabolites following rectal and intravenous administration in dogs. N Z Vet J. 2009 Jun;57(3):146-52.
7 Benitez ME, Roush JK, KuKanich B, McMurphy R. Pharmacokinetics of hydrocodone and tramadol administered for control of postoperative pain in dogs following tibial plateau leveling osteotomy. Am J Vet Res. 2015 Sep;76(9):763-70. doi: 10.2460/ajvr.76.9.763.
8 Itami T, Tamaru N, Kawase K, Ishizuka T, Tamura J, Miyoshi K, Umar MA, Inoue H, Yamashita K. Cardiovascular effects of tramadol in dogs anesthetized with sevoflurane. J Vet Med Sci. 2011 Dec;73(12):1603-9.
9 Itami T, Kawase K, Tamaru N, Ishizuka T, Tamura J, Miyoshi K, A Umar M, Inoue H, Yamashita K. Effects of a Single Bolus Intravenous Dose of Tramadol on Minimum Alveolar Concentration (MAC) of Sevoflurane in Dogs. J Vet Med Sci. 2013 Jan 7. [Epub ahead of print]
10 Martins TL, Kahvegian MA, Noel-Morgan J, et al. Comparison of the effects of tramadol, codeine, and ketoprofen alone or in combination on postoperative pain and on concentrations of blood glucose, serum cortisol, and serum interleukin-6 in dogs undergoing maxillectomy or mandibulectomy. Am J Vet Res. 2010 Sep;71(9):1019-26
11 Seddighi MR, Egger CM, Rohrbach BW, et al. Effects of tramadol on the minimum alveolar concentration of sevoflurane in dogs. Vet Aneaesth Analg. 2009 Jul;36(4):334-40
12 Vettorato E. Zonca A, Isola M, et al. Pharmacokinetics and efficacy of intravenous and extradural tramadol in dogs. Vet J. 2010 Mar;183(3):310-5
13 Kongara K, Chambers JP, Johnson CB. Effects of tramadol, morphine or their combination in dogs undergoing ovariohysterectomy on perioperative electroencephalographic responses and post-operative pain. N Z Vet J. 2012 Mar;60(2):129-35.
14 Kongara K, Chambers JP, Johnson CB, Dukkipati VS. Effects of tramadol or morphine in dogs undergoing castration on intra-operative electroencephalogram responses and post-operative pain. N Z Vet J. 2013 Feb 28. [Epub ahead of print]
15 Morgaz J, Navarrete R, Muñoz-Rascón P, Domínguez JM, Fernández-Sarmiento JA, Gómez-Villamandos RJ, Granados MM. Postoperative analgesic effects of dexketoprofen, buprenorphine and tramadol in dogs undergoing ovariohysterectomy. Res Vet Sci. 2013 Aug;95(1):278-82.
16 Malek S, Sample SJ, Schwartz Z, Nemke B, Jacobson PB, Cozzi EM, Schaefer SL, Bleedorn JA, Holzman G, Muir P. Effect of analgesic therapy on clinical outcome measures in a randomized controlled trial using client-owned dogs with hip osteoarthritis. BMC Vet Res. 2012 Oct 4;8(1):185.
17 Matthiesen T, Wöhrmann T, Coogan TP, Uragg H. The experimental toxicology of tramadol: an overview. Toxicol Lett. 1998 Mar 16;95(1):63-71.
18 Malek S, Sample SJ, Schwartz Z, Nemke B, Jacobson PB, Cozzi EM, Schaefer SL, Bleedorn JA, Holzman G, Muir P. Effect of analgesic therapy on clinical outcome measures in a randomized controlled trial using client-owned dogs with hip osteoarthritis. BMC Vet Res. 2012 Oct 4;8:185.
19 Kukanich B, Papich MG. Pharmacokinetics and antinociceptive effects of oral tramadol hydrochloride administration in Greyhounds. Am J Vet Res 2011 Feb;72(2):256-62
20 Flôr PB, Yazbek KV, Ida KK, Fantoni DT. Tramadol plus metamizole combined or not with anti-inflammatory drugs is clinically effective for moderate to severe chronic pain treatment in cancer patients. Vet Anaesth Analg. 2013 May;40(3):316-27.
21 Davila D, Keeshen TP, Evans RB, Conzemius MG. Comparison of the analgesic efficacy of perioperative firocoxib and tramadol administration in dogs undergoing tibial plateau leveling osteotomy. J Am Vet Med Assoc. 2013 Jul 15;243(2):225-31.
22 Rialland P, Authier S, Guillot M, Del Castillo JR, Veilleux-Lemieux D, Frank D, Gauvin D, Troncy E. Validation of orthopedic postoperative pain assessment methods for dogs: a prospective, blinded, randomized, placebo-controlled study. PLoS One. 2012;7(11):e 49480.
23 Lascelles, BDX, Adjunctive Therapy for Canine Osteoarthritis (S26C), Proceedings Western Veterinary Conference 2007.
24 Pypendop BH, Ilkiw JE. Pharmacokinetics of tramadol, and its metabolite O-desmethyl-tramadol, in cats. J Vet Pharmacol Ther. 2008 Feb;31(1):52-9.
25 Pypendop BH, Siao KT, Ilkiw JE. Effects of tramadol hydrochloride on the thermal threshold in cats. Am J Vet Res. 2009 Dec;70(12):146570.
26 Brondani JI, Loureiro Luna SP, Beier SL et al. Analgesic efficacy of perioperative use of vedaprofen, tramadol or their combination in cats undergoing ovariohysterectomy. J Feline Med Surg. 2009 Jun;11(6):420-9
27 Ray J, Jordan D, Pinelli C, Fackler B, Boggess D, Clark J. Case studies of compounded Tramadol use in cats. Int J Pharm Compd. 2012 JanFeb;16(1):44-9.
32
Budsberg SC, Torres BT, Kleine SA, Sandberg GS, Berjeski AK. Lack of effectiveness of tramadol hydrochloride for the treatment of pain and joint dysfunction in dogs with chronic osteoarthritis. J Am Vet Med Assoc. 2018 Feb 15;252(4):427-432.
29 Donati PA, Tarragona L, Franco JVA, Kreil V, Fravega R, Dias A, Verdier N, Otero P. Efficacy of tramadol for postoperative pain management in dogs: systematic review and meta-analysis. Review Vet Anaesth Analg. 2021 May;48(3):283-296.
30 Food & Drug Administration Freedom of Information, http://www.accessdata.fda.gov/drugsatfd ... rmR_P2.pdf p. 60-62
31 Therapeutic Goods Administration, http://www.tga.gov.au/pdf/auspar/auspar-palexia.pdf p. 9
32 Giorgi M, Meizler A, Mills PC. Pharmacokinetics of the novel atypical opioid tapentadol following oral and intravenous administration in dogs. Vet J. 2012 Jul 6. [Epub ahead of print]
33 Koegel, B, Terlinden R, Schneider J. Characterisation of tramadol, morphine and tapentadol in an acute pain model in Beagle dogs. Gruenenthal GmbH, 2012
34 Lee HK, Lebkowska-Wieruszewska B, Kim TW, Kowaski CJ, Giorgi M. Pharmacokinetics of the novel atypical opioid tapentadol after intravenous, intramuscular and subcutaneous administration in cats. Vet J. 2013 Dec;198(3):620-4.
35 Longmire DR, Jay GW, Boswell MV. Neuropathic Pain. In: Weiner’s Pain Management, A Practical Guide for Clinicians, 7th ed. Boswell MV, Cole BE ed. Taylor & Francis, Boca Raton FL 2006, p. 305.
36 Solak O, Metin M, et al, Effectiveness of gabapentin in the treatment of chronic post-thoracotomy pain, Eur J Cardiothorac Surg. 2007 Jul;32(1):9-12. Epub 2007 Apr 17
37 Ahn SH, Park HW. Gabapentin effect on neuropathic pain compared among patients with spinal cord injury and different durations of symptoms. Spine. 2003 Feb 15;28(4):341-6; discussion 346-7
38 Rowbotham M, Harden M. Gabapentin for the treatment of postherpetic neuralgia: a randomized controlled trial. JAMA 1998 Dec 2;280(21):1837-42
39 Backonja M, Glanzman RL. Gabapentin dosing for neuropathic pain: evidence from randomized, placebo-controlled clinical trials. Clin Ther. 2003 Jan;25(1):81-104
40 Lascelles BDX. Drug therapy for acute and chronic pain the cat. Int J Pharm Compounding 2002;6:338-343.
41 Plessas IN, Rusbridge C, Driver CJ, Chandler KE, Craig A, McGonnell IM, Brodbelt DC, Volk HA. Long-term outcome of Cavalier King Charles spaniel dogs with clinical signs associated with Chiari-like malformation and syringomyelia. Vet Rec. 2012 Nov 17;171(20):501.
42 Wolfe KC, Poma R. Syringomyelia in the Cavalier King Charles spaniel (CKCS) dog. Can Vet J. 2010 Jan;51(1):95-102.
43 Rusbridge C, Heath S, Gunn-Moore DA, Knowler SP, Johnston N, McFadyen AK. Feline orofacial pain syndrome (FOPS): a retrospective study of 113 cases. J Feline Med Surg. 2010 Jun;12(6):498-508.
44 Lu Y, Westlund K. Gabapentin Attenuates Nociceptive Behaviors in an Acute Arthritis Model in Rats JPET 290:214–219, 1999
45Hanesch U, et al Gabapentin reduces the mechanosensitivity of fine afferent nerve fibres in normal and inflamed rat knee joints. Pain. 2003 Jul;104(1-2):363-6
46 Boileau et al, Oral treatment with PD-0200347, an alpha2delta ligand, reduces the development of experimental osteoarthritis by inhibiting metalloproteinases and inducible nitric oxide synthase gene expression and synthesis in cartilage chondrocytes, Arthritis Rheum 2005 Feb; 52(2):488-500
47 Plessas IN, Rusbridge C, Driver CJ, Chandler KE, Craig A, McGonnell IM, Brodbelt DC, Volk HA.
Long-term outcome of Cavalier King Charles spaniel dogs with clinical signs associated with Chiari-like malformation and syringomyelia. Vet Rec. 2012 Nov 17;171(20):501.
48 Wolfe KC, Poma R. Syringomyelia in the Cavalier King Charles spaniel (CKCS) dog. Can Vet J. 2010 Jan;51(1):95-102.
49 Cashmore RG, Harcourt-Brown TR, Freeman PM, Jeffery ND, Granger N. Clinical diagnosis and treatment of suspected neuropathic pain in three dogs. Aust Vet J. 2009 Jan-Feb;87(1):45-50
50 Hélène LMR, Watanabe R, Evangelista, MC, Beauchamp G, Steagall PV. Analgesic Effects of Gabapentin Alone or in Combination with Meloxicam in Dogs with Neuropathic Pain, Univ Montreal 2019
51 Clare Rusbridge1, Sarah Heath, Danièlle A Gunn-Moore, Susan Penelope Knowler, Norman Johnston, Angus Kennedy McFadyen. Feline orofacial pain syndrome (FOPS): a retrospective study of 113 cases. J Feline Med Surg. June 2010;12(6):498-508.
52 Troncy E, personal communication 2013
53 Lorenz ND, Comerford EJ, Iff I. Lorenz 2012: Long-term use of gabapentin for musculoskeletal disease and trauma in three cats. J Feline Med Surg. 2012 Dec 19.
54 Hurley RW, Cohen SP, et al, The analgesic effects of perioperative gabapentin on postoperative pain: a meta-analysis. Reg Anesth Pain Med 2006 May-Jun;31(3):237-47
55 Ho, Gan TJ, Habib AS.. Gabapentin and postoperative pain a systematic review of randomized controlled trials.Pain. 2006 Dec 15;126(13):91-101. Epub 2006 Jul 18
56 Tippana Hamunen K, Kontinen VK, Kalso E. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg. 2007 Jun;104(6):1545-56
57 Seib RK, Paul JE. Preoperative gabapentin for postoperative analgesia: a meta-analysis. Can J Anaesth. 2006 May;53(5):461-9.
58 Clivatti J, Sakata RK, Issy AM. Review of the use of gabapentin in the control of postoperative pain. Rev Bras Anestesiol. 2009 JanFeb;59(1):87-98.
59 Doleman B, Heinink TP, Read DJ, Faleiro RJ, Lund JN, Williams JP. A systematic review and meta-regression analysis of prophylactic gabapentin for postoperative pain. Anaesthesia. 2015 Oct;70(10):1186-204.
60 Reid P, Pypendop BH, Ilkiw JE.The Effects of Intravenous Gabapentin Administration on the Minimum Alveolar Concentration of Isoflurane in Cats. Anesth Analg. 2010 Jun 14.
61 Wagner AE, Mich PM, Uhrig SR, Hellyer PW. Clinical evaluation of perioperative administration of gabapentin as an adjunct for postoperative analgesia in dogs undergoing amputation of a forelimb. J Am Vet Med Assoc. 2010 Apr 1;236(7):751-6.
62 Aghighi SA, Tipold A, Piechotta M, Lewczuk P, Kästner SB. Assessment of the effects of adjunctive gabapentin on postoperative pain after intervertebral disc surgery in dogs. Vet Anaesth Analg. 2012 Nov;39(6):636-46.
63 Pypendop BH, Siao KT, Ilkiw JE. Thermal antinociceptive effect of orally administered gabapentin in healthy cats. Am J Vet Res. 2010 Sep;71(9):1027-32.
64 Crociolli GC, Cassu RN, Barbero RC, Rocha TL, Gomes DR, Nicácio GM. Gabapentin as an adjuvant for postoperative pain management in dogs undergoing mastectomy. Med Sci. 2015 Aug;77(8):1011-5. 33
28
65 Lorenz ND, Comerford EJ, Iff I. Lorenz 2012: Long-term use of gabapentin for musculoskeletal disease and trauma in three cats. J Feline Med Surg. 2012 Dec 19. [Epub ahead of print]
66 Kukanich B, Cohen RL Pharmacokinetics of oral gabapentin in greyhound dogs. Vet J. 2009 Oct 22
67Vollmer KO, Parmacokinetics and metabolism of gabapentin in rat, dog and man, Arzneimittelforschung, 1986; 36(5):830-9
68 Radulovic LL, Türck D, von Hodenberg A, et al. Disposition of gabapentin (neurontin) in mice, rats, dogs, and monkeys. Drug Metab Dispos. 1995 Apr;23(4):441-8.
69 Siao KT, Pypendop BH, Ilkiw JE. Pharmacokinetics of gabapentin in cats. Am J Vet Res. 2010 Jul;71(7):817-21.
70 Schmidt PC, Ruchelli G, Mackey SC, Carroll IR. Perioperative gabapentinoids: choice of agent, dose, timing, and effects on chronic postsurgical pain. Anesthesiology. 2013 Nov;119(5):1215-21.
71 Salazar V, Dewey CW, Schwark W, Badgley L, Gleed RD, Horne W, Ludders JW. Pharmacokinetics of single-dose oral pregabalin administration in normal dogs. Vet Anaesth Analg. 2009 Nov;36(6):574-80.
72 Plessas IN, Rusbridge C, Driver CJ, Chandler KE, Craig A, McGonnell IM, Brodbelt DC, Volk HA. Long-term outcome of Cavalier King Charles spaniel dogs with clinical signs associated with Chiari-like malformation and syringomyelia. Vet Rec. 2012 Nov 17;171(20):501.
73 Plumb’s Veterinary Drug Handbook, 5th ed. Plumb DC, Blackwell Publishing Limited, 2005
74 Fisher K, Coderre TJ, Hagen NA. Targeting the N-methyl-D-aspartate receptor for chronic pain management. Preclinical animal studies, recent clinical experience and future research directions. J Pain Symptom Manage 2000;20:358-373.
75 Collins S, Sigtermans MJ, Dahan A, Zuurmond WW, Perez RS. NMDA receptor antagonists for the treatment of neuropathic pain. Pain Med. 2010 Nov;11(11):1726-42.
76 Lascelles BDX, Gaynor J, Smith ES. Evaluation of Amantadine as Part of a Multimodal Analgesic Regimen for the Alleviation of Refractory Canine Osteoarthritis Pain, WORLD SMALL ANIMAL VETERINARY ASSOCIATION WORLD CONGRESS PROCEEDINGS, 2007
77 Madden M, Gurney M, Bright S. Amantadine, an N-Methyl-D-Aspartate antagonist, for treatment of chronic neuropathic pain in a dog. Vet Anaesth Analg. 2014 Jul;41(4):440-1
78 Norkus C, Rankin D, Warner M, KuKanich B. Pharmacokinetics of oral amantadine in greyhound dogs. J Vet Pharmacol Ther. 2015 Jun;38(3):305-8.
79 Vernier VG, Harmon JB, Stump JM, et al. The toxicologic and pharmacologic properties of amantadine hydrochloride. Toxicol Appl Pharmacol 1969;15:642-665
80 Siao KT, Pypendop BH, Stanley SD, Ilkiw JE. Pharmacokinetics of amantadine in cats. J Vet Pharmacol Ther. 2011 Dec;34(6):599-604.
81 Cao X, Nakamura Y, Wada T, Izumi-Nakaseko H, Ando K, Sugiyama A. Electropharmacological effects of amantadine on cardiovascular system assessed with J-Tpeak and Tpeak-Tend analysis in the halothane-anesthetized beagle dogs. J Toxicol Sci. 2016;41(3):439-47.
82 Longmire DR, Jay GW, Boswell MV, Neuropathic Pain, In: Weiner’s Pain Management, A Practical Guide for Clinicians, 7th ed. Boswell MV, Cole BE ed. Taylor & Francis, Boca Raton FL 2006, p. 306-7.
83 Finnerup NB et al, Algorithm for neuropathic pain treatment: an evidence based proposal, Pain 2005: 118:289-305
84 Cashmore RG, Harcourt-Brown TR, Freeman PM, Jeffery ND, Granger N. Clinical diagnosis and treatment of suspected neuropathic pain in three dogs. Aust Vet J. 2009 Jan-Feb;87(1):45-50
85 Chew DJ, Buffington CA, Kendall MS, et al. Amitriptyline treatment for severe recurrent idiopathic cystitis in cats. J Am Vet Med Assoc 1998;213:1282-1286.
86KuKanich B. Outpatient Oral Analgesics in Dogs and Cats: Beyond Nonsteroidal Antiinflammatory Drugs: An Evidence-based Approach, in Vet Clin Small Anim 43 (2013) 1109–1125
87 http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Scientific_Discussion/human/000572/WC500036776.pdf
88 Baek IH, Lee BY, Kang W, Kwon KI. doi: 10.1055/s-0033-1341493. Epub 2013 Apr 18.
Pharmacokinetic analysis of two different doses of duloxetine following oral administration in dogs. Drug Res (Stuttg). 2013 Aug;63(8):404-8.
89 Sullivan M, Bentley S, Fan MY, Gardner G. A single-blind placebo run-in study of venlafaxine XR for activity-limiting osteoarthritis pain. Pain Med. 2009 Jul-Aug;10(5):806-12.
90 Howell SR, Hicks DR, Scatina JA, Sisenwine SF. Pharmacokinetics of venlafaxine and O-desmethylvenlafaxine in laboratory animals. Xenobiotica. 1994 Apr;24(4):315-27.
91 Belinskaia DA, Belinskaia MA, Barygin OI, Vanchakova NP, Shestakova NN. Psychotropic Drugs for the Management of Chronic Pain and Itch. Pharmaceuticals (Basel). 2019 Jun 24;12(2).
92 Neil MJ. Clonidine: clinical pharmacology and therapeutic use in pain management. Curr Clin Pharmacol. 2011 Nov;6(4):280-7.
93 Lebkowska-Wieruszewska B, De Vito V, Owen H, Poapholatep A, Giorgi M. Pharmacokinetics of grapiprant, a selective EP4 prostaglandin PGE2 receptor antagonist, after 2 mg/kg oral and i.v. administrations in cats. J Vet Pharmacol Ther. 2017 Dec;40(6):e11-e15
94 Rausch-Derra LC, Rhodes L. Safety and toxicokinetic profiles associated with daily oral administration of grapiprant, a selective antagonist of the prostaglandin E2 EP4 receptor, to cats. Am J Vet Res. 2016 Jul;77(7):688-92.
95 De Vito V, Salvadori M, Poapolathep A, Owen H, Rychshanova R, Giorgi M. Pharmacokinetic/pharmacodynamic evaluation of grapiprant in a carrageenan-induced inflammatory pain model in the rabbit. J Vet Pharmacol Ther. 2017 Oct;40(5):468-475.
96 Budsberg SC, Kleine SA, Norton MM, Sandberg GS. Comparison of two inhibitors of E-type prostanoid receptor four and carprofen in dogs with experimentally induced acute synovitis. Am J Vet Res. 2019 Nov;80(11):1001-1006.
97 de Salazar AG, Gioda L, Dehman A, Beugnet F. Assessment of the efficacy of firocoxib (Previcox®) and grapiprant (Galliprant®) in an induced model of acute arthritis in dogs. BMC Vet Res. 2019 Aug 29;15(1):309.
98 Chandrasekharan NV, Dai H, Roos KL, et al. COX3, a COX1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad sci USA 2002 Oct 15;99(21):13926-31.
99 Mburu DN, Mbugua SW, Skoglund LA, Lökken P. Effects of paracetamol and acetylsalicylic acid on the post-operative course after experimental orthopaedic surgery in dogs. J Vet Pharmacol Ther 988;11(2):163-170.
100 Mburu, DN.. Evaluation of the anti-inflammatory effects of a low dose of acetaminophen following surgery in dogs. Vet Pharmacol. 1991 14:109-11
101 KuKanich B. Pharmacokinetics of acetaminophen, codeine, and the codeine metabolites morphine and codeine-6-glucuronide in healthy Greyhound dogs. J Vet Pharmacol Ther. 2010 Feb;33(1):15-21.
34
102 Neirinckx E, Vervaet C, De Boever S, et al. Species comparison of oral bioavailability, first-pass metabolism and pharmacokinetics of acetaminophen. Res Vet Sci. 2010 Aug;89(1):113-9.
103 Savides MC, Oehme FW, Nash SL, Leipold HW. The toxicity and biotransformation of single doses of acetaminophen in dogs and cats. Toxicol Appl Pharmacol. 1984 Jun 15;74(1):26-34.
104 KuKanich B. Pharmacokinetics and pharmacodynamics of oral acetaminophen in combination with codeine in healthy Greyhound dogs. J Vet Pharmacol Ther. 2016 Oct;39(5):514-7.
105 Sikina ER, Bach JF, Lin Z, Gehring R, KuKanich B. Bioavailability of suppository acetaminophen in healthy and hospitalized ill dogs. J Vet Pharmacol Ther. 2018 May 13. doi: 10.1111/jvp.12664. [Epub ahead of print]
106 McConkey SE, Grant DM, Cribb AE. The role of para-aminophenol in acetaminophen-induced methemoglobinemia in dogs and cats. J Vet Pharmacol Ther. 2009 Dec;32(6):585-95.
107 Savides MC, Oehme FW, Nash SL, Leipold HW. The toxicity and biotransformation of single doses of acetaminophen in dogs and cats. Toxicol Appl Pharmacol. 1984 Jun 15;74(1):26-34.
108 Schlesinger DP. Methemoglobinemia and anemia in a dog with acetaminophen toxicity. Can Vet J. 1995 Aug;36(8):515-7.
109 MacNaughton SM. Acetaminophen toxicosis in a Dalmatian. Can Vet J. 2003 Feb; 44(2):142-4.
110 Wallace KP, Center SA, Hickford FH, Warner KL, Smith S. S-adenosyl-L-methionine (SAMe) for the treatment of acetaminophen toxicity in a dog. J Am Anim Hosp Assoc. 2002 May-Jun;38(3):246-54.
111 Harvey JW, French TW, Senior DF. Hematologic abnormalities associated with chronic acetaminophen administration in a dog. JAm Vet Med Assoc. 1986 Nov 15;189(10):1334-5.
112 Kim PS, Fishman MA. Low-Dose Naltrexone for Chronic Pain: Update and Systemic Review. Curr Pain Headache Rep. 2020 Aug 26;24(10):64.
113 Machado MC, da Costa-Neto JM, Portela RD, Melhor MJ, D’Assis H, Martins-Fhilho OA,, Barrouin-Melo SM, da Costa-Neto JM, Borges NF, Silva FL, Estrela-Lima A. The effect of naltrexone as a carboplatin chemotherapy-associated drug on the immune response, quality of life and survival of dogs with mammary carcinoma. PLoS One. 2018 Oct 4;13(10):e0204830..
35
Parenteral Medications for the Chronic Pain Management
36
Parenteral Medications for the Chronic Pain Patient
Mark Epstein DVM, DABVP (C/F), CVPP
TotalBond Veterinary Hospitals
Gastonia & Charlotte, NC USA
International Veterinary Academy of Pain Management
Introduction
It can be argued that chronic pain is the most ubiquitous disease process in all of medicine. All animals, whether human and veterinary should they live long enough, will probably experience it. And of all chronic pain syndromes, osteoarthritis (OA) remains the most predictable cause in both dogs and cats. Indeed, in dogs the pathophysiology of OA is commonly heritable and conformational, to include, joint incongruity, joint malalignment, and intrinsic cartilaginous defects. For these dogs, the disease process begins at a very young age and is progressive and lifelong. At least 30-40% of dogs may be affected clinically, 1 with a higher percentage (up to 60%) having radiographic changes associated with degenerative joint disease. 2 Other common causes include acquired conditions such as trauma, including not insignificantly chronic cranial cruciate ligament (CCL) injury and acute-on-chronic CCL rupture. Nearly half of musculoskeletal disorders identified during a 10-year span in 16 veterinary hospitals resulted from joint disease. 3 The etiology of OA in cats is uncertain, with less attributable to conformation (exception: hip dysplasia in Maine Coons 4) than dogs. Cats, both young and old, appear to have a very high incidence of OA, with up to 60% of all cats have radiographic OA changes and 90% over 10 years old. 5 Although the pathophysiology of OA may be different in dogs and cats, this means that OA in both these species can initiate early in life, far earlier (relatively speaking) than routinely in humans, and how we intervene in OA may be quite different from one life stage to another.
Other categories of chronic pain include cancer pain (e.g. especially osteosarcoma or any bone-related neoplasia) and non-OA, non-cancer pain (e.g. chronic neuropathic pain conditions such as feline hyperesthesia syndrome, lymphoplasmacytic stomatitis/gingivitis, persistent post-surgical – especially post-amputation – pain, and many more).
Outside the realm of NSAID and opioid exist a broad range of medications that exert an analgesic effect, or otherwise modify and protect against pain, by manipulating various targets a long the nociceptive pathway. This session will focus on those medications administered by the parenteral route.
KETAMINE
A phencyclidine dissociative anesthetic ketamine exerts a pain-modifying effect predominantly as potent NMDA-receptor antagonist. Ketamine binds to its receptor inside the NMDA receptor, i.e. the calcium channel would already have to be open and active for ketamine to exert its effect. However, once bound, it decreases the channel’s opening time and frequency, thus reducing Ca+ ion influx and dampening secondary intracellular signaling cascades. Hence it is unlikely (and has not been shown) to be truly analgesic in nature. Rather, subanesthetic ketamine constant rate infusion (CRI) has been shown convincingly in humans to have pain-preventive, anti-hyperalgesic, anti-allodynic effects 6 , 7 , 8 , 9 , 10 , 11 , 12 and appears also to play a role in minimizing the neuropathic phenomenon of Persistent Post-Surgical Pain (PPSP). 13 Existing studies in the dog appear to suggest similar clinical effects in dogs 14 , 15 , 16 (not yet studied in a feline surgical model). Consensus Guidelines in humans advocate the use of ketamine CRI in patient populations where the degree of post-surgical pain would be expected to be severe, and generally as an opioid-sparing modality. 17 The International Veterinary Academy of Pain Management and the 2015 American Animal Hospital Association – American Association of Feline Practitioners Pain
37
Management Guidelines have both adopted a position that the pain-modifying effects and safety warrant the consideration of subanesthetic ketamine as part of a multi-modal approach to transoperative pain management, especially in patients with risk factors that may dispose them to exaggerated or maladaptive pain states. Such conditions include, but are not limited to:
• Any nerve or neuron injury
• Severe trauma (pre-existing and/or intra-operative)
• Pre-existing long-standing inflammation (e.g. osteoarthritis)
• Use of neurotoxic agents (e.g. certain chemotherapeutics e.g. vincristine)
A customary dosing schedule can be described as follows:
Ketamine HCl 60 mg (0.6 ml of 100 mg/ml product) is placed in 1 L of crystalloid fluids (= 60 mg/L), administered at a customary surgical fluid rate of 5-10 ml/kg/hr (depending in blood and/or insensible fluid loss), delivering 5-10 mcg/kg/min. Post-operatively reduce to maintenance rate of 2 ml/kg/hr, delivering 2 mcg/kg/min. Protocols generally describe a loading dose of 0.25 – 0.5 mg/kg ketamine IV bolus at initiation of the CRI; induction anesthetic doses may (should) be lowered accordingly.
Consensus Guidelines in humans also suggest a role for ketamine CRI in the case of patients with chronic maladaptive, neuropathic pain syndromes, although without a unifying dosing or administration schedule recommendation. 18
BISPHOSPHONATES
Administered by IV infusion, the class of drug exerts anti-osteoclast activity and can contribute to pain sustained (weeks) pain-modifying effect in approximately 80% of dogs with osteosarcoma. The protocol described is 1 – 2 mg/kg; diluted into 250 mL of 0.9% sodium chloride and administered as a CRI over 2 hours every 28 days; monitor renal values before each infusion. 19 Zolendronate is now generic, decreases lameness in 75% of dogs, and is more renal friendly; it is administered 0.1mg/kg IV in 60 ml saline over 15min every 4 weeks (still check renal values prior to each infusion).
POLYSULFATED GLYCOSAMINOGLYCANS
Parenterally-administered PSGAG products have regulatory approval as safe and effective chondroprotectants, supported by independent studies. 20 , 21 , 22 Although not an analgesic drug per se, a clinical effect can be said to be conferred by minimizing the release of pro-inflammatory cytokines (e.g. IL1, PGE2) and degradative enzymes (e.g. metalleoproteinases). Adequan™ (Luitpold) is labeled in dogs for 4.4 mg/kg IM twice weekly for 4 weeks. However, extra-label long-term use is commonly employed, generally administered once monthly and adjusting frequency according to patient needs. Extra-label use also includes administering subcutaneously instead of IM; bioavailability is thought to be similar, which is supported by a study of radio-labeled SC administration in cats Heidrich 2008 VOS 23. Use in cats with DJD is also extra-label but anecdotally appears effective in this species as well.
Pentosan polysulphate is labeled in the U.K., Canada (Catrophen-Vet®), and Australia (Arthropen-Vet®) as an injectable chondroprotectant, 3 mg/kg SC once weekly for 4 weeks. Extralabel uses would be in the U.S., in cats, and chronically.
Anti-NGF MAb
Originally identified for its role in embryonic development of the nervous system, Nerve Growth Factor (NGF) is now known to have the ability to alter the function of nociceptors in the adult. NGF is upregulated in inflamed tissues, binds to Trk-A receptors on nociceptor endings there, and contributes to pain and peripheral sensitization.
38
Microglial cells in the dorsal horn of the spinal cord constitute a significant source of NGF which can be induced into excess production under circumstances of glial activation (see below), thus also contributing to central hypersensitization.
NGF is responsible for several physiologic aberrations of pain processing: this includes but is not limited to sprouting of terminal nerve endings and thus promoting “cross-talk” between numbers and types of neurons that ordinarily would not have been involved in pain processing (creates the circumstance of expanded field of pain, and the experience of hyperalgesia and allodynia).
Several different NGF-antagonism strategies have been explored, and at least 4 companies working to develop specifically an anti-NGF monoclonal antibody product for humans suffering from OA, low back pain, and cancer pain. FDA Phase II, III trials for OA were conducted for the molecules tanezumab, fulranumab, REGN475. In 2010 efficacy in reducing pain was established but several individuals developed Rapidly Progressing Osteoarthritis (RPOA, a phenomenon that occurs naturally in humans but not described in dogs or cats); a disproportionate number of trial subjects developing RPOA were also taking NSAID. The trials were halted, but in 2012 the FDA authorized continuation of trials with narrowed patient inclusion criteria, excluding the use of NSAID. Veterinary therapeutic anti-NGF MAb products are in developmental stages, utilizing a patented the technology (PETisation™) that enables rapid translation of mouse or human proteins for the treatment of other species (caninization 24, felinization 25). Initial efficacy data appears encouraging for 1 month of pain-modifying effect in canine 26 and feline 27 OA after subcutaneous administration. In 2022, Solensia™ was FDA approved and launched for monthly administration in cats, and in May 2023, LIbrela™ was similarly approved in dogs.
Intra-Articular injections for OA – some commercially available, others investigational
1. Stem Cells (autologous mesenchymal vs. allogeneic) 28 , 29
2. Platelet-rich Plasma (PRP) 30 , 31
3. Stromal-vascular fraction 32
4. Autologous Protein Solution 33
5. Tn-117 – Commercially available anti-synovitis medical device (Synovetin OA™)
6. Resiniferotxin – TRPV1 agonist under investigation 34 (“molecular neurosurgery”)
1 Johnson JA, Austin C, Bruer GJ. Incidence of Canine Appendicular Musculoskeletal Disorders in 16 Veterinary Teaching Hospitals from 1980 through 1989. Vet Compar OrthTrauma, 1994 (7): 56-69.
2 Bland SD. Canine osteoarthritis and treatments: a review. Vet Sci Dev, 43 Refs ed. 2015 Vol 5 (2) pp. 5931, 84-89.
3 JA, Austin C, Breur GJ. Incidence of canine appendicular musculoskeletal disorders in 16 veterinary teaching hospitals from 1980 through 1989. Johnson Vet Comp Orthop Trauma 7:56-69, 1994.
4 Loder RT, Todhunter RJ. Demographics of hip dysplasia in the Maine Coon cat. J Feline Med Surg. 2018 Apr;20(4):302-307.
5 Lascelles BD, Henry JB 3rd, Brown J, Robertson I, Sumrell AT, Simpson W, Wheeler S, Hansen BD, Zamprogno H, Freire M, Pease A Cross-sectional study of the prevalence of radiographic degenerative joint disease in domesticated cats. Vet Surg. 2010 Jul;39(5):535-44.
6 Ketamine: Does Life Begin at 40? IASP Pain Clinical Updates, Carr DB, ed. XV:3, June 2007
7 Richebe P, et al. Low doses ketamine: antihyperalgesic drug, non-analgesic. Ann Fr Anesth Reanim. 2005 Nov-Dec;24(11-12):1349-59
8 MCartney CJ et al. A qualitative systematic review of the role of N-methyl-D-aspartate receptor antagonists in preventive analgesia. Anesth Analg. 2004 May;98(5):1385-400
9Subramaniam K et al. Ketamine as adjuvant analgesic to opioids: a quantitative and qualitative systematic review. Anesth Analg. 2004 Aug;99(2):482-95
10 Bell RF et al. Perioperative ketamine for acute postoperative pain. Cochrane Database Syst Rev. 2006 Jan 25;(1)
11 Elia N, Tramer MR. Ketamine and postoperative pain a quantitative systematic review of randomised trials. Pain. 2005 Jan;113(1-2):61-70
12 Brinck EVC, Tiippana E, Heesen M, Bell RF, Straube S, Moore RA, Kontinen V.
Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst Rev. 2018 Dec; 2018(12): CD012033
13 McNicol ED, Schumann R, Haroutounian S. A systematic review and meta-analysis of ketamine for the prevention of persistent postsurgical pain. Acta Anaesthesiol Scand. 2014 Nov;58(10):1199-213.
39
14 Slingsby LS, Waterman-Pearson AE, The postoperative analgesic effects of ketamine after canine ovariohysterectomy – a comparison between pre- and post-operative administration. Res Vet Sci. 2000 Oct;69(2):147-52
15 Sarrau S, Jourdan J, Dupuis-Soyris F, Verwaerde P. Effects of postoperative ketamine infusion on pain control and feeding behaviour in bitches undergoing mastectomy. J Small Anim Pract. 2007 Dec;48(12):670-6.
16Wagner AE, Walton JA, Hellyer PW, Gaynor JS, Mama KR. Use of low doses of ketamine administered by constant rate infusion as an adjunct for postoperative analgesia in dogs. J Am Vet Med Assoc. 2002 Jul 1;221(1):72-5.
17 Schwenk ES, Viscusi ER, Buvanendran A, Hurley RW, Wasan AD, Narouze S, Bhatia A, Davis FN, Hooten WM, Cohen SP. Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Acute Pain Management From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018 Jul;43(5):456-466.
18 Cohen SP, Bhatia A, Buvanendran A, Schwenk ES, Wasan AD, Hurley RW, Viscusi ER, Narouze S, Davis FN, Ritchie EC, Lubenow TR, Hooten WM. Consensus Guidelines on the Use of Intravenous Ketamine Infusions for Chronic Pain From the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018 Jul;43(5):521-546.
19Fan TM, et al. Evaluation of intravenous pamidronate administration in 33 cancer-bearing dogs with primary or secondary bone involvement. J Vet Intern Med. 2005 Jan-Feb;19(1):74-80.
20 Fujiki M, Shineha J, Yamanokuchi K, Misumi K, Sakamoto H. Effects of treatment with polysulfated glycosaminoglycan on serum cartilage oligomeric matrix protein and C-reactive protein concentrations, serum matrix metalloproteinase-2 and -9 activities, and lameness in dogs with osteoarthritis. Am J Vet Res. 2007 Aug;68(8):827-33.
21 Altman RD, Howell DS, Muniz OE, Dean DD. The effect of glycosaminoglycan polysulfuric acid ester on articular cartilage in experimental arthritis: effects on collagenolytic enzyme activity and cartilage swelling properties. J Rheumatol. 1987 May;14 Spec No:127-9.
22 Lust G, Williams AJ, Burton-Wurster N, Beck KA, Rubin G. Effects of intramuscular administration of glycosaminoglycan polysulfates on signs of incipient hip dysplasia in growing pups. Am J Vet Res. 1992 Oct;53(10):1836-43.
23 Heidrich JE, Fox SM, Royer R, Vanderjagt D, Doyle S, Tokars M. Fluoresceine-labeled polysulfated glycosaminoglycan in a feline Acute traumatic knee model. Veterinary Orthopedic Society Proceedings, 2008.
24 Gearing DP, Virtue ER, Gearing RP, Drew AC. A fully caninised anti-NGF monoclonal antibody for pain relief in dogs. BMC Vet Res. 2013 Nov 9;9:226.
25 Gearing DP, Huebner M, Virtue ER, Knight K, Hansen P, Lascelles BD, Gearing RP, Drew AC. In Vitro and In Vivo Characterization of a Fully Felinized Therapeutic Anti-Nerve Growth Factor Monoclonal Antibody for the Treatment of Pain in Cats. J Vet Intern Med. 2016 Jul;30(4):1129-37.
26 Lascelles BD, Knazovicky D, Case B, Freire M, Innes JF, Drew AC, Gearing. A canine-specific anti-nerve growth factor antibody alleviates pain and improves mobility and function in dogs with degenerative joint disease-associated pain. BMC Vet Res. 2015 Apr 30;11:101.
27 Gruen ME, Thomson AE, Griffith EH, Paradise H, Gearing DP, Lascelles BD. A Feline-Specific Anti-Nerve Growth Factor Antibody Improves Mobility in Cats with Degenerative Joint Disease-Associated Pain: A Pilot Proof of Concept Study. J Vet Intern Med. 2016 Jul;30(4):1138-48.
28 Vilar JM1, Batista M, Morales M, Santana A, Cuervo B, Rubio M, Cugat R, Sopena J, Carrillo JM. Assessment of the effect of intraarticular injection of autologous adipose-derived mesenchymal stem cells in osteoarthritic dogs using a double blinded force platform analysis. BMC Vet Res. 2014 Jul 1;10:143.
29 Vilar JM, Morales M, Santana A, Spinella G, Rubio M, Cuervo B, Cugat R, Carrillo JM. Controlled, blinded force platform analysis of the effect of intraarticular injection of autologous adipose-derived mesenchymal stem cells associated to PRGF-Endoret in osteoarthritic dogs. BMC Vet Res. 2013 Jul 2;9:131.
30 Upchurch DA, Renberg WC, Roush JK, Milliken GA, Weiss ML. Effects of administration of adipose-derived stromal vascular fraction and platelet-rich plasma to dogs with osteoarthritis of the hip joints. Am J Vet Res. 2016 Sep;77(9):940-51.
31 Vilar JM, Manera ME, Santana A, Spinella G, Rodriguez O, Rubio M, Carrillo JM, Sopena J, Batista M. Effect of leukocyte-reduced platelet-rich plasma on osteoarthritis caused by cranial cruciate ligament rupture: A canine gait analysis model. PLoS One. 2018 Mar 19;13(3):e0194752.
32 Marx C, Silveira MD, Selbach I, da Silva AS, Braga LM, Camassola M, Nardi NB. Acupoint injection of autologous stromal vascular fraction and allogeneic adipose-derived stem cells to treat hip dysplasia in dogs.
33 Wanstrath AW, Hettlich BF, Su L, Smith A, Zekas LJ, Allen MJ, Bertone AL. Evaluation of a Single Intra-Articular Injection of Autologous Protein Solution for Treatment of Osteoarthritis in a Canine Population. Vet Surg. 2016 Aug;45(6):764-74.
34 Iadarola MJ, Sapio MR, Raithel SJ, Mannes AJ, Brown DC. Long-term pain relief in canine osteoarthritis by a single intra-articular injection of resiniferatoxin, a potent TRPV1 agonist. Pain. 2018 Oct;159(10):2105-2114.
40
Speaker Biography
 Elizabeth Rozanski, DVM, DACVECC, DACVIM (SAIM)
Elizabeth Rozanski, DVM, DACVECC, DACVIM (SAIM)
Dr. Elizabeth Rozanski graduated from the University of Illinois with her DVM degree. After completing a residency in Philadelphia, she joined Tufts University, drawn in by the position's combination of research, teaching, and service. She teaches toxicology and respiratory medicine throughout the four-year Cummings School DVM curriculum. As a member of the Foster Hospital for Small Animals' emergency and critical care team, Dr. Rozanski treats animals at one of the nation's busiest academic emergency rooms. She is board-certified in both internal medicine and emergency and critical care and is the past president of the Veterinary Comparative Respiratory Society.
Dr. Elizabeth Rozanski
CVMA Fall Seminar- October 6-8, 2023
41
Brachycephalics: The Worst Is Yet to Come
42
Brachycephalics: The Worst Is Yet to Come
Elizabeth Rozanski, DVM, DACVIM (SA-IM), DACVECC Tufts University School of Veterinary Medicine
Respiratory diseases as well as respiratory distress are common complaints in dogs. Due to unique breed characteristics, including anatomic features, there is a breed predilection for many conditions. In no case is this more evident than in dogs with brachycephalic (BC) confirmation. BC dogs are prone to a variety of conditions associated with chronic hypoxemia and increased intra-thoracic pressures including not only respiratory obstruction, but also heatstroke, gastrointestinal disease, and heart-based tumors. Some evidence supports as well an increased tendency towards hypercoagulability and some dogs have a syndrome that is similar to sleep apnea.
Respiratory
Upper airway obstruction is a common and occasionally under-recognized source of respiratory distress. As an overview, dogs with upper airway obstruction will have noisy breathing that worsens with exercise or heat exposure. Normal inspiration results in negative pressure inside the upper airways, which causes collapse of weaker or less supported tissues. Recurrent obstruction contributes to tissue swelling and edema, which further magnifies obstruction. Heat stress, which leads to panting, is associated with higher inspiratory flow rate, which may require more work of breathing due to partial airway obstruction, which results more muscle activity and paradoxically further overheating. Specific upper airway disease includes brachycephalic obstructive airway syndrome (BAS), and laryngeal paralysis. Rhinitis may also contribute to airway obstruction, as dogs are preferential nasal breathers, particularly at rest. The brachycephalic dog, and the bulldog in particular are particularly affected with upper airway obstruction.
All bulldogs have some component of BAS. Classic features include stenotic nares, long/thick soft palate, everted laryngeal saccules, tracheal hypoplasia, and in some dogs laryngeal collapse or nasopharyngeal turbinates. (1,2) Pharyngeal edema and collapse may also occur with prolonged obstruction.
Treatment of bulldogs includes early conversation with the owners of bulldogs, and consideration for surgical palliation with soft palate resection and/or stenotic nares resection.
(2)Many owners assume exercise intolerance and stertorous breathing are normal, and may be reassured that surgery will typically result in marked improvement in quality of life, particularly if performed early in life.
Long-standing obstruction will result in increased pharyngeal soft tissue weakness, and may potentially result in less improvement after palliative surgery than if done earlier in life.
43
Surgical palliation may be successfully performed in practice by the interested clinician or by a surgeon, either using a laser or hand-suturing techniques. (2). Permanent tracheostomy may be required in severely affected dogs. (figure 1)
Pneumonia is adult brachycephalic dogs is usually due to aspiration. Aspiration may be sterile (e.g. Chemical) but more classically appears to be bacterial. Bulldog puppies are also commonly affected with community-acquired pneumonia, particularly when shipped in a long distance.
Treatment of aspiration/bacterial pneumonia requires first the clinical recognition. Common signs include lethargy, cough, tachypnea or respiratory distress and occasionally nasal discharge. Routine thoracic radiographs will document alveolar infiltrate, most common in the right middle lung. Severe pneumonia may affect all lung lobes, while early changes may be primarily interstitial in nature. As in all radiographic interpretation it is wise to completely evaluate the ribs, sternum, pleural space, cardiac silhouette as well as any areas of the neck or abdomen that are visible. Bulldogs in particular may have tracheal hypoplasia, which may impact clearance in pneumonia.
Broad spectrum antibiotics, ideally based upon culture and sensitivity testing are advised. Collection of samples for airway washes may be challenging in brachycephalics; transtracheal washes are typically hard to successful obtain in BC dogs, so transoral washes are preferable. Pending culture results, good combinations include enrofloxacin and ampicillin or Cefazolingentamicin-metronidazole. Other combinations are certainly acceptable as well, as long as there is adequate gram-positive, gram-negative and anaerobic coverage. Other essential care includes intravenous fluids for hydration, and supplemental oxygen if shortness of breath is present. Oxygen therapy is useful to reduce the work of breathing, improve patient comfort (e.g. Decrease air hunger) and improve tissue oxygenation. The duration of antibiotic therapy is dependent on clinical course. In veterinary medicine, some clinicians advocate treatment for 4 weeks at least, plus until evidence of radiographic resolution of the infiltrates. In human medicine, treatment duration tends to be shorter; this may ultimately be advisable for our patients as well.
Anesthetic complications
Brachycephalic dogs are prone to anesthetic concerns, specifically difficulty with regurgitation and extubation. In general, while intubated these dogs are happy! However, during recovery, vomiting or regurgitation may be common due to swallowed air, and airway swelling may accompany intubation. Guidelines for bulldogs include: Fasting to avoid a full stomach and pre-treatment with metoclopramide (Reglan) is wise. For elective surgery, pre-treatment with omeprazole is ideal if possible.
44
Intubation requires a good light sources, and ideally to have success confirmed with end-tidal CO2 assessment. The tube should be maintained for as long as possible post operatively and the BC should not be left to recover unobserved. (Figure 2)
Hospital acquired distress
Bulldogs and other brachycephalics are also very prone to decompensation in the hospital due to the stress of hospitalization and occasionally handling. Excessive stertor should be treated before airway obstruction develops and all lay staff should additionally be educated on upper airway disease.
Cardiac disease
Bulldogs are also predisposed to two type of cardiovascular disease, the first being arrhythmogenic right ventricular cardiomyopathy (ARVC); this is similar to the boxer cardiomyopathy, where often more of the disease reflects ectopy, rather than myocardial dysfunction. Bulldogs are notoriously hard to auscultate due to upper airway sounds, and thoracic radiographs are hard to interpret. Treatment Bulldogs (and other BC breeds) are also prone to the development of heart-based tumors (not hemangiosarcoma) which may result in exercise intolerance or syncope for compression of the pulmonary artery or pericardial effusion. X-rays will again be hard to interpret, and jugular venous distension is hard to appreciate in a bulldog. Diagnosis is by echocardiography.
Heat stress and gastrointestinal disease
Bulldogs are also prone to heat stress due to their inability to effectively cool and also are prone to gastrointestinal distress and esophageal dysfunction. GI distress may be reflective of aerophagia and intermittent hiatal hernias. (3,4) Chronic therapy with a proton pump inhibitor, such as omeprazole (1 mg/kg or 20 mg/bulldog) may be helpful and can be considered in all bulldogs. Avoidance of obesity is also useful with many bulldogs benefitting from specific veterinary diet input to avoid maintaining extra weight.
Summary of Diagnostic techniques- A complete medical history and physical examination should be performed prior to sedated diagnostics in brachycephalic dogs. The location of disease or suspected disease should be established. For diagnostic testing that requires anesthesia or sedation, if possible, it is prudent to combine surgical or other palliative therapy with those diagnostics and avoid the “wake up and make plan”, especially for patients with compromised upper airways.
45
The major diagnostic testing options available
1) Thoracic radiographs- Radiographs are most helpful for dogs with suspected lower airway disease (eosinophilic bronchitis), pneumonia and pulmonary fibrosis as diagnostic tools, are useful to evaluate for concurrent pneumonia or hiatal hernia in bulldogs.
2) Computed tomography – Primary use is identification of pulmonary fibrosis. A lung biopsy is definitive, but less commonly performed due to costs, potential risks and current lack of therapeutic options.
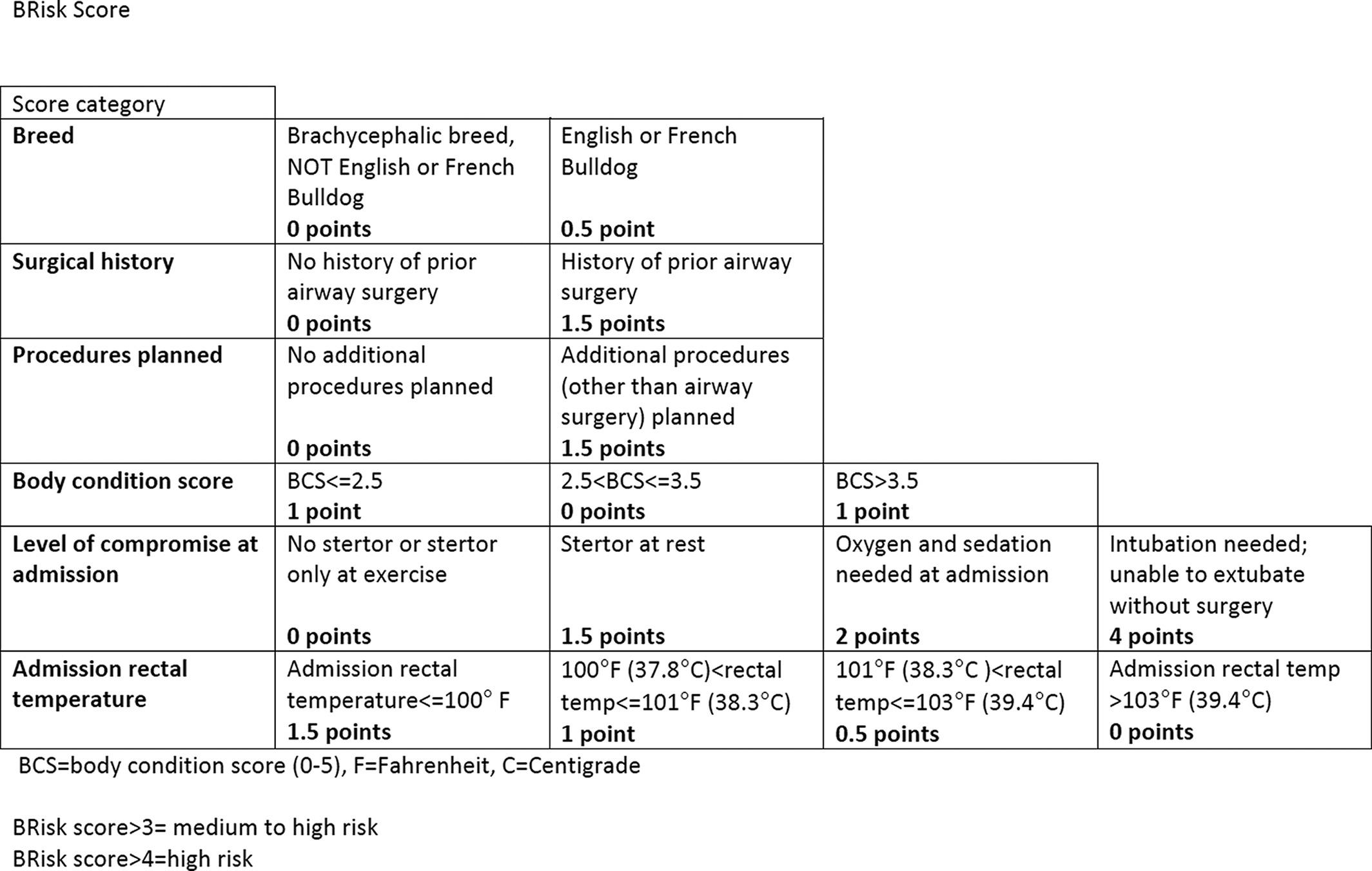
3) Oral examination- Most useful in dogs with upper airway disease; Doxapram (1-2 mg/kg IV) may be useful to identify any dynamic collapse.
4) Bronchoscopy- Useful in tracheal collapse or tracheal hypoplasia
5) Airway cytology and culture- Useful for eosinophilic disease and excluding or establishing bacterial infections. Recall that colonization is common in the lower airways and a positive culture does not necessarily indicate infection.
New developments include the BRISK Score
OFA clearance- New 2023
https://www.avma.org/news/health-screening-test-rolled-out-brachycephalic-dog-breeds
46
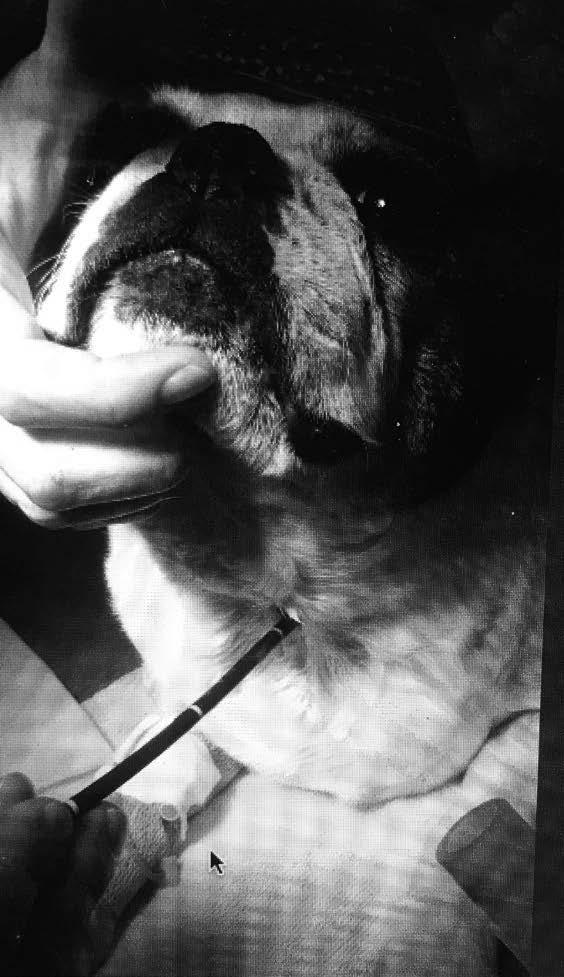
 Figure 1
Figure 1
47
Figure 2.
References
1) Riecks TW, Birchard SJ, Stephens JA. Surgical correction of brachycephalic syndrome in dogs: 62 cases (1991-2004). J Am Vet Med Assoc. 2007 May 1;230(9):1324-8
2) Ginn JA, Kumar MS, McKiernan BC, Powers BE Nasopharyngeal turbinates in brachycephalic dogs and cats.J Am Anim Hosp Assoc. 2008 Sep-Oct;44(5):243-9.
3) Poncet CM, Dupre GP, Freiche VG, et al. Long-term results of upper respiratory syndrome surgery and gastrointestinal tract medical treatment in 51 brachycephalic dogs.J Small Anim Pract. 2006 Mar;47(3):137-42.
4) Poncet CM, Dupre GP, Freiche VG et al. Prevalence of gastrointestinal tract lesions in 73 brachycephalic dogs with upper respiratory syndrome. J Small Anim Pract. 2005 Jun;46(6):273-9.
5) Johnson LR, Mayhew PD, Steffey MA et al. Upper airway obstruction in Norwich Terriers: 16 cases. J Vet Intern Med. 2013 Nov-Dec;27(6):1409-15.
48
It Is Not Always Bad! 49
Feline Respiratory Distress:
Feline Respiratory Distress: It Is Not Always Bad!
Elizabeth Rozanski, DVM, DACVIM (SA-IM), DACVECC Tufts Cummings School of Veterinary Medicine
Respiratory distress in cats is common and challenging. Cats often compensate well for pulmonary diseases, and some conditions can rapidly fulminate. It is crucial to balance the equal goals of limiting stress on the cat with respiratory distress, and to work to identify the specific cause of the distress so that appropriate therapy can be provided.
Phone triage- Home care of the cat with respiratory distress is not advised. Cats with respiratory distress should be evaluated by a veterinarian as soon as possible. Cats with known pre-existing therapy may receive additional therapy at home immediately before leaving to come to the hospital, such as an additional dose of furosemide to a known heart failure cat, or albuterol/terbutaline and prednisone to a known lower airway disease cat.
Initial examination and stabilization-Initial physical examination should focus on the major body systems (heart, brain and lungs) and include an assessment of respiratory rate and effort, with a specific focus on evaluation increased airway sounds, or dull/absent sounds with increased effort. Auscultation of the heart may document a murmur or gallop, although it should be recalled that that murmurs may be hard to hear in the ER at times. Rectal temperature should be recorded, as hypothermia is common in cats with congestive heart failure. Following rapid assessment, supplemental oxygen should be provided, and a history obtained from the cat’s family. Most cats with respiratory distress do not have remarkably revealing histories, but care should be taken to inquire about past diagnosis (including auscultation of a heart murmur), possible trauma/exposure to the outdoors, and any other changes, such as decreased appetite, cough (or suspected “hairballs”) or PU/PD. Following a brief physical examination and assessment of the cat’s medical history, an initial attempt at therapy should be provided, including continuing oxygen therapy, diuretics, glucocorticoids, or thoracocentesis. In a growing number of hospitals, ultrasonography (US) is readily available. Used of US is vital for rapid assessment of pleural effusion with minimal training, with more advanced training and practice, other assessments, such as left atrial size, evidence of LV hypertrophy, or mediastinal masses may also be provided. In my experience, the use of ultrasound has largely negated the need to perform a “diagnostic” thoracocentesis, and limits unnecessary discomfort to cats, and eliminates the possibility of iatrogenic pneumothorax.
Thoracic radiographs are ultimately required to (well at least HELP..) determine the cause of respiratory distress in most cats. Ideal positioning is NOT required when cats are in respiratory distress. It may be wise to start with a single view, and then to allow the cat to recover for a few minutes before taking a second view.
A standard approach to interpretation of the thoracic radiograph includes evaluation of the pulmonary parenchyma, the pleural space, the cardiac silhouette, ribs and diaphragm.
50
Tips for evaluation of chest film include
1) When looking for pleural effusion, small volumes will obscure the lung/diaphragm interface on a DV or VD projection.
2) Cardiomegaly may be subtle, even in fulminate heart failure.
3) Patchy infiltrates are most often heart failure.
4) Bronchial disease can look like metastatic disease.
5) Rib fractures can accompany coughing/respiratory distress.
6) If films look normal, consider upper airway disease.
Other diagnostic testing may include echocardiography, pleural effusion cytology, transoral tracheal wash, and/or computed tomography. A reasonable overview is to try to determine “heart or not heart” and then pursue diagnostic testing from there. In our ER less than 50% of cats with respiratory distress have heart failure, so it is wise to keep an open mind as to the potential causes, including consideration of a) upper airway disease b) lower airway disease c) Parenchymal disease d) pleural space disease or e) trickery. Hypoventilation may cause hypoxemia or hypercarbia, but these will not be easily appreciated on physical examination.
DISORDERS TO BE FAMILIAR WITH
UPPER AIRWAY: Nasopharyngeal polyps- Young cats, with loud stridor/stertor, occasionally dysphagia. Direct visualization on oral examination, removal with traction or ventral bulla osteotomy. Nasopharyngeal stenosis- narrowing of NP, treat with balloon or stent. Laryngeal paralysis- cats may be clinical with unilateral paresis, maybe idiopathic or due to tumor/infection etc. May be managed medically or surgically (avoid if possible!) Laryngeal masses- usually squamous cell carcinoma, may be benign. Specific therapy dependent on underlying condition.
LOWER AIRWAY: Feline asthma, which implies reversible bronchoconstriction and chronic bronchitis are common disorders. Infection, such as mycoplasma may also result in respiratory disease. Therapy is currently directed towards addressing the underlying irritant and then longterm prednisone.
PARENCHYMAL DISEASE: Congestive heart failure, typically from cardiomyopathy may result in pulmonary edema. This may appear patchy in distribution. Pro-NT BNP testing has been recently introduced and may be helpful in identifying cats at risk of CHF or in CHF. Infection is rare in adult cats, but may occasionally occur in kittens or due to atypical organisms (eg. Toxoplasmosis), and finally neoplasia (metastatic or primary) may occur in cats as well. Pulmonary contusions may also result parenchymal infiltrates. Recall that severe bronchial disease may look like metastatic disease.
PLEURAL EFFUSION: May represent congestive heart failure, pyothorax, chylothorax or neoplasia (specifically lymphoma). Pleural effusion is a sign, not a final diagnosis. Other pleural space diseases (“parasites”) include pneumothorax (spontaneous or traumatic), diaphragmatic hernia, or neoplasia.
51
Therapeutic approach to respiratory distress in best directed at the “best guess” of the underlying disease process. Specific tips that are important to consider for evaluating cats with respiratory distress are:
1) Iatrogenic pneumothorax is very common following thoracocentesis in cats with longstanding effusions. Pleural effusion leads to the thickening of the pleura, and this if nicked, will continue to leak air. Recall that normal lung seals quickly.
2) Old cats don’t get new onset asthma. Airway disease in cats is a young to middle age cat disease. Cats may cough their entire lives, but barring lifestyle changes (e.g. moving to a different climate or with a smoker) they should not develop cough as geriatric cats.
3)Cold cats have heart failure. While admitably, cats may be hard to “temp” if they are stressed, cats that are hypothermic are very commonly in heart failure.
4)Cats that eat well in oxygen are hyperthyroid or have neoplastic disease. Anorexia is common in the stressed/short of breath cat, and finding a cat who is truly devouring the offered food, makes the likelihood of cancer or hyperthyroidism higher.
5) NT pro BNP is super helpful.
6)Bronchial disease may appear similar to mets.
7)Rounded lung lobes, suggest chronic effusion, and increase the risk for pneumothorax.
Cat 1
History: 4-year-old Maine Coon type cat. Has been hiding more for the last few days. Now short of breath
Physical Examination: Labored breathing, Temp 98.7 intermittent gallop
Cat 2
History: 17-year-old cat, had toe abscess a few weeks, now breathing hard. Had been on Clavamox.
Physical Examination: Increased effort, muffled lung sounds, thin, toe still looks infected.
52
Cat 3
History: 15-year-old cat, wheezing acute onset two weeks ago. Starting prednisone, but no improvement
Physical Examination: Loud airway sounds, 3/6 murmur
Cat 4
History: 4-year cat, acutely can’t use back legs. Eats a vegan diet
Physical Examination: Temp 97 degrees, HR 180, RR 60, no femoral pulses, Gallop
Cat 5
History: Owner’s daughter is a veterinary tech, noticed mom’s cat breathing hard. Mom didn’t notice anything.
Physical Examination: Overweight, increased effort, pleural effusion which looks like cream when tapped
53
The Airway Is Your Air-Emy
54
The Airway Is Your Air-Emey
Elizabeth Rozanski, DVM, DACVIM, DACVECC Cummings School of Veterinary Medicine
The Unified Airway Concept (UAC) refers to the idea that human patients with chronic airway disease are more likely to have both upper and lower airway disease. This observation may be useful for understanding the pathogenesis of airways diseases, and equally importantly may be helpful in improving treatment as treating all locations of disease may be more likely to improve the clinical signs. It is unknown of this overlap occurs in cats and dogs, but it a novel concept that should be more completely explored in veterinary patients. Specifically, the two most common overlapping disease syndromes we will consider here include the 1) Asthma: chronic rhinosinusitis syndrome (CRS) in cats and 2) Bronchiectasis and rhinosinusitis in dogs. In order to best understand how the airway inflammation develops, it is important to recognize that the airway can react to stimuli in a limited number of ways, including airway edema, excessive mucus production epithelial damage and inflammation and ultimately fibrotic changes. Airway epithelium’s normal function is to defend the lung against invasion by irritants and microrganisms. Chronic allergic airway disease is thought to represent an over-enthusiastic response to a substance (allergy) which results in the influx of eosinophils, which further perpetuate airway inflammation and edema. In veterinary medicine, respiratory disease may represent allergy or inflammation; there is not always a clear distinction between irritant, neutrophilic and eosinophilic inflammation. Additionally, of some interest, at least in dogs, it is hard to induce cough through aerosol inhalants. In order to better consider the potential consequences of these overlapping conditions, it is wise to consider the traditional clinical evaluation of these respiratory conditions.
Cats

Nasal disease is frequently observed in cats, with the major differential diagnoses include nasal tumor, Cryptococcus, dental disease, foreign body and chronic rhinosinusitis. CRS is a disease of immense frustration to veterinarian, owners and likely cats. Chronic inflammation leads to excessive mucus production and destruction of the nasal turbinates. The diagnostic approach to a cat with CRS includes a complete physical examination, which is usually unremarkable other than nasal disease as well as diagnostic testings. Laboratory testing, including FeLV testing is warranted, as immunosuppression has been associated with development of Cryptococcus. Nasal culture, while commonly performed, is almost never truly helpful, as primary bacterial sinusitis is almost never documented, but rather secondary colonization. Figure 1A showed an MRI scan of a cat with severe chronic rhinitis, with destruction of turbinates, while figure 1B shows a normal nose. Treatment of nasal disease is more effective when directed at the primary cause While CRS may be limited to the nose, cough may also develop in response to post nasal drip or possible due to concurrent lower airway disease. Antibiotic therapy is often beneficial to limit nasal discharge, but is not curative. Antiinflammatory therapy may help some cats, including prednisone or NSAIDs(with caution). Antihistamines are occasionally helpful, although not as much as in people for reasons that are not entirely clear, but likely reflect both differences in disease as well species difference in the role of histamine.
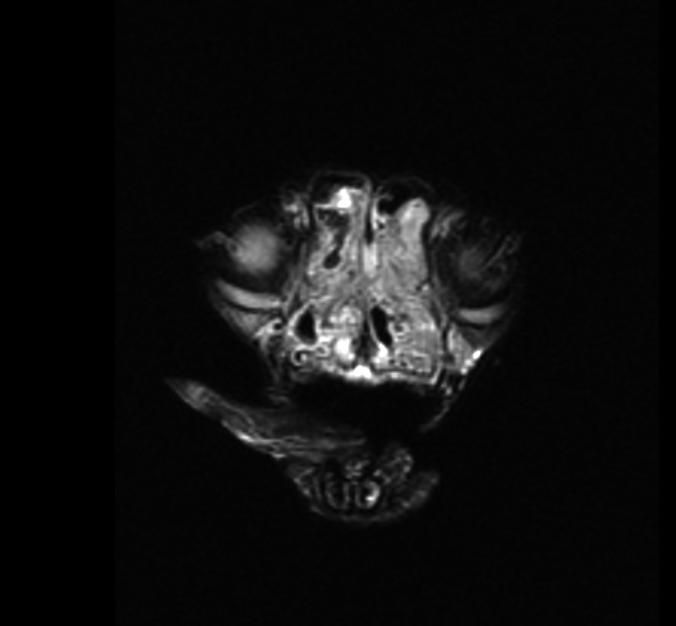
55
Figure 1A (left side, shows a cat with severe turbinate destruction secondary to chronic rhinitis, while Figure 1B shows normal sinuses.
Lower airway disease is commonly suspected in cats with cough, and/or respiratory distress. The underlying cause surrounding the development of lower airway disease remained undetermined in most cats. Siamese cats have been described as over-represented with lower airway disease, but it is unclear if this is a real increase or if Siamese cats may be more likely to present for on-going veterinary care. Viral respiratory infections are a common cause of asthma in genetically susceptible infants and children. While viral respiratory infections are common in kittens, it is unclear the role that respiratory infections may have in the development of later lower airway disease in cats. Prior viral upper respiratory tract infection DO predispose cats to chronic upper respiratory diseases (e.g. Rhinotracheitis/herpes) Lower airway disease is suspected to represent allergy to some inhaled allergen in most cases, but how/why a specific cat becomes sensitized remains unclear. Some cats appear to worsen seasonally, while others appear to have year-round disease. Certain cats appear to react to dustier kitty litters, or the presence of indoor pollution, including environmental tobacco smoke or potpourris. Allergy testing is rarely performed in cats with suspected asthma, but one pilot study in cats showed a high rate of positive responses to skin testing. Experimentally, cats may be sensitized to various antigens, such as Bermuda grass (Reinero Lab, Missouri) or A. suum (Several European universities) and a clinical syndrome similar to lower airway diseases may be stimulated with re-exposure. Thoracic radiographs are a mainstay of diagnosis, which affected cats demonstrating a bronchial or bronchointerstital pattern. Cats may also have hyperinflation due to airtrapping and occasionally collapse of the right middle lung lobe due to mucus plugging. Recall that older cats don’t typically develop airway disease, and cough in a geriatric patient should be carefully evaluate to exclude other causes. A pulmonary tumor causing cough in an older cat is shown in figure 3.

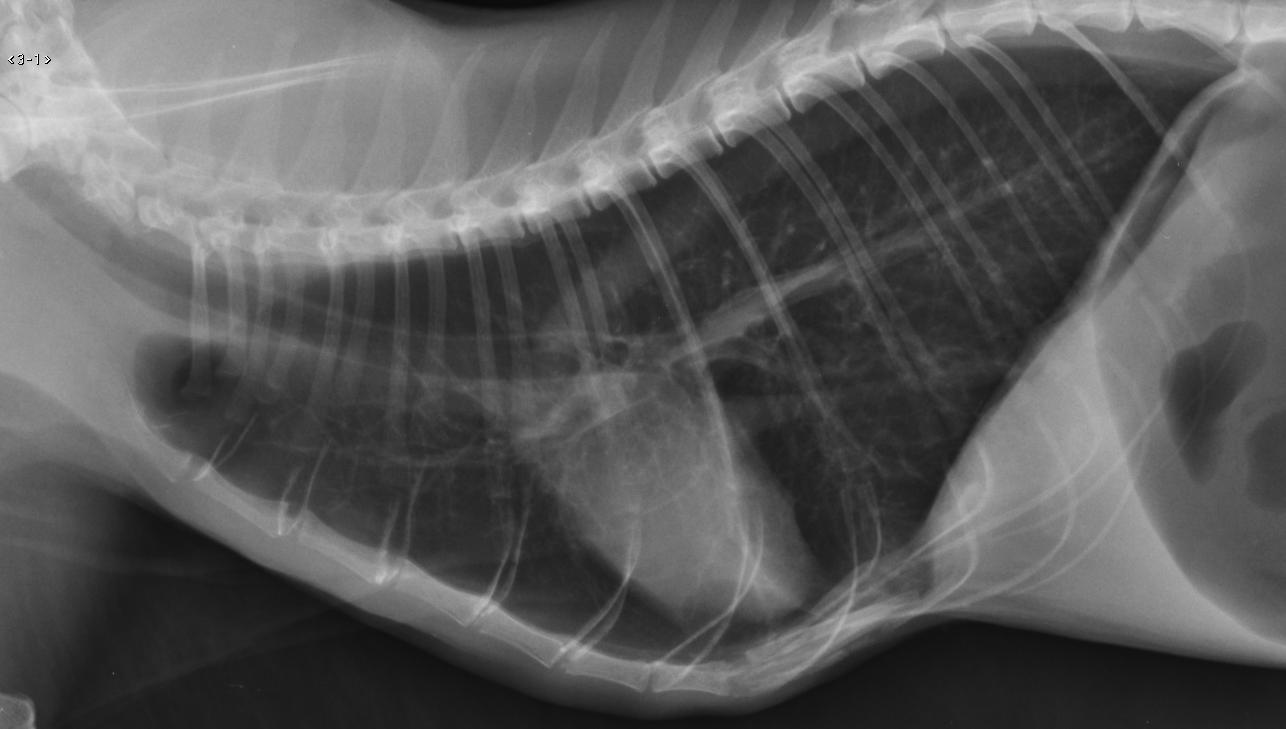
Treatment of confirmed asthma/lower airway disease includes in the acute setting includes supplemental oxygen therapy, glucocorticoids and bronchodilators while more chronic therapy includes removing any identifiable trigger, and glucocorticoids. Other therapeutic options, such as stem cells, or desensitization may become available in the coming years for both airway disease and rhinitis.
In human medicine, complete evaluation of the patient with respiratory signs includes a complete evaluation of signs of allergic rhinitis in the asthma patient and of asthma signs in the rhinitis patient. Of crucial difference in cats, a complete evaluation of each patient may not always be performed, and moreover, owner may not be able to easily difference the origin of the clinical signs. For veterinarians,
Figure 2 lateral radiograph from a cat with severe lower airway disease. Note in specific the hyperinflation, and bronchial pattern.
Figure 3. Note the pulmonary mass in the caudal dorsal lung field.
56
the goal of this discussion is to recognize that airway changes may extend over the length of the respiratory epithelium, and care should be taken in cats with CRS to ask about cough, and in cats with primarily lower airway disease to consider the rate of upper airway signs. The potential role of chronic viral infections as a cause for both upper and lower airway disease in cats is an exciting area for investigation. It is well-recognized that viral infection in human infants may lead to the development of asthma and chronic allergic rhinitis. Cats are also commonly affected by viral respiratory infections although it may be hard to know the entire history of an individual cat, particularly those adopted as adults.
Chronic bronchitis (CB) is a lower airway inflammatory disease, characterized by predominantly neutrophilic infiltrates and much less eosinophilia. Clinical signs of chronic bronchitis include frequent cough on most or all days over the preceding two months in which a more specific cause (e.g. Cancer, heart failure) has been excluded. CB is most common in small older breed dogs. There has been limited to no evidence that allergy results in the development of chronic bronchitis. Dogs with chronic bronchitis may sneeze and/or have nasal discharge, this may reflect nasal aspiration of expectorated bronchial secretions and subsequent inflammation or may reflect primary rhinitis.
In people, in addition to a relationship between asthma and chronic rhinitis, there has also been recognized a relationship between bronchiectasis and rhinitis/nasal polyps. Bronchiectasis is a complication of chronic bronchitis, where the lower airways enlarge and may become filled with purulent material. Bronchiectasis is considered part of the COPD complex in people, which includes chronic bronchitis and emphysema. In dogs, emphysema is recognized rarely although chronic bronchitis is common and bronchiectasis may develop in more chronically affected dogs. Bronchiectasis is typically appreciated as complication of bronchitis or bronchopneumonia and may be seen as a dilated airway on radiograph or CT analysis. Bronchiectasis does require periodic treatment with antibiotics and in fact some studies in people suggest that daily treatment with azithromycin reduces the number of exacerbations requiring hospitalization. Nasal polyps are very uncommon in dogs, so this relationship may be hard to further explore.
SUMMARY
In people, the concept of a unified airway, with signs of upper and lower inflammatory or allergic disease being recognized with increasing frequency. It is prudent in cats and dogs that present with signs that initially localize to nasal or lower airways to be vigilant about inquiring about other respiratory signs. Treatment of the entire airway should result in better outcome as well as further our understanding of these common syndromes.
References
1) Corren JJ Allergy Clin Immunol. Allergic rhinitis and asthma: how important is the link? 1997 Feb;99(2):S781-6.
2) Guilemany JM1, Angrill J, Alobid I et al. United airways again: high prevalence of rhinosinusitis and nasal polyps in bronchiectasis. Allergy. 2009 May;64(5):790-7
3) Reed N. Chronic rhinitis in the cat. Vet Clin North Am Small Anim Pract. 2014 Jan;44(1):33-50
4) Scherk M Snots and snuffles: rational approach to chronic feline upper respiratory syndromes.J Feline Med Surg. 2010 Jul;12(7):548-57.
5) Hawkins E.C., Clay L.D., Bradley J.M., et al. Demographic and Historical Findings, Including Exposure to Environmental Tobacco Smoke, in Dogs with Chronic Cough. J Vet Intern Med 2010; 24: 825-831.
6) Padrid P.A., Hornof W.J., Kurpershoek C.J., et al. Canine Chronic Bronchitis: A Pathophysiologic Evaluation of 18 Cases. J Vet Intern Med 1990; 4: 172-180
57
The Geriatric Pet in the ER
58
The Geriatric Pet in the ER
Elizabeth Rozanski, DVM, DACVECC, DACVIM Tufts University School of Veterinary Medicine
Geriatric pets make up a large percentage of cases that are seen on urgent or emergent basis. Clearly, most older pets are part of the family for an extended length of time, and any illness or injury may be met with more profound emotional responses than for younger pets where the family is less likely to have life or death decisions. As with all families, with healthy older pets it can be reasonable to develop a “living will”; where the family discusses ahead of time what their companion becomes ill. Specifically, it may be useful to explain that typical causes of death in older animals include organ failure, cancer, and severe arthritis.
Initial guideline for phone triage of older pets should include more aggressive advice to have the patient evaluated. While a young Labrador might tolerate a day or two of vomiting without complications, an older dog may not be able to tolerate dehydration without progressive decline in renal function. Owners should obviously be encouraged to have a close relationship with their primary care veterinarian. There is less evidence of exactly what is age-appropriate screening tests, but in general physical examination at least yearly and at any point where there is evidence of disease. Baseline laboratory tests are warranted if possible, at the very least assessing hematocrit, creatinine and liver enzymes. Patients on chronic medications, including NSAIDs, should be more regularly evaluated. Some owners and clinicians are keen to more completely evaluate patients; individualized screening tests may be indicated for certain patients or recommended as a hospital policy Emerging screening testing include NT-pro BNP for cardiac disease in both cats and dogs, and SDMA for early detection of renal disease. More specialized testing may only be available at certain reference laboratories (e.g. IDEXX versus Antech, versus local reference lab). As with all testing, it is prudent to have a plan as what you might do with a positive result in an asymptomatic patient.
Frailty
Concept of FRAIL is important to discuss in relation to older pets. Frailty is a concept that is widespread in people, and had just begun to be evaluated in dogs and cats. Frailty refers in people to the syndrome associated with unintentional weight loss, lack of energy, lack of strength, slow gait and low activity. Frailty in people is associated with increasing risk of death, and longer hospitalization times. In animals, while frail dogs and cats are regularly seen, the impact of this aging in outcomes in cats and dogs is less well-recognized.
Emergency presentations for geriatric pets can be divided several ways. One easy way to divide them is to separate new presentations from presentations for progression of pre-existing disease. As with all emergencies, prompt triage (assessment for evidence of abnormalities with the heart, brain or lungs) is warranted even in the family thinks it is clear what the problem is.
Pre-existing disease
Common pre-existing disease that may worsen include:
Renal failure- Patients with renal disease may present with worsening azotemia, typically magnified by vomiting, anorexia and dehydration. This may be termed acute on chronic renal failure. The major points for managing worsening renal function include replacing any hydration deficits, and evaluating for evidence of urinary tract infection. Emerging trends in renal medicine are recognizing that the goals for fluid therapy is to replace deficits and to ensure adequate hydration. There is no specific benefit to extra fluids and diuresis alone is not beneficial to improving kidney function.
59
Congestive heart failure- CHF is common in small breed dogs due to valvular disease, and in larger dogs with DCM. Cats commonly have hypertrophic cardiomyopathy. Urgent assessment includes determining the need for more diuretics or other increased therapies, and/or determining in azotemia is present. Heart disease is progressive, but the time frame can be variable, as can the response to therapy. Diet history (particularly salty foods) is warranted, and consideration for additional therapies if heart failure has worsened, or decreased diuretics if azotemia is more a concern than respiratory distress. Pulmonary disease Pulmonary diseases that may exacerbate include tracheal collapse/chronic bronchitis syndrome, as well as laryngeal paralysis and polyneuropathy complex in larger dogs. Heat stress may magnify these conditions, as well as secondary infections.
Arthritis –Arthritis may appear to acutely worsen, but in most cases, there is actually a slow progression of disease, where one day the pet appears much worse, although to the veterinarian, the dog is far worse than at the last visit. Infection (either septic joint or urinary tract) may also result in worsening of the lameness. Additionally, pathologic fractures may occur in association most typically with osteosarcoma.
Cancer- Prior diagnosis of cancer may or may not be relevant in the treatment of the older pet; some cancers (e.g. Grade I mast cell tumors) are effectively surgically cured, while other cancers may have recurrent or metastatic complications. Owners that have previously treated a pet for cancer may be more inclined to pursue further therapy.
Neurological disease- Late onset seizures in dogs is more often indicative of systemic disease or brain tumor/
Acute collapse
Acute collapse in older dogs commonly represents bleeding, most typically in to the abdomen (e.g. Splenic mass) or pericardium. Point of care ultrasound (POCUS) has tremendously improved the ability of primary care practices to urgently detect hemorrhage/ fluid into body cavities. All older animals with collapse should be evaluated for internal hemorrhage or pericardial effusion. Classical clinical signs include anemia without hypoproteinemia (due to acute loss) for hemoabdomen, and pulsus paradoxus with pericardial effusion. Importantly, many of the older dogs with hemoabdomen have a recent clinical history of PU/PD for a few days or resolved lethargy, likely associated with smaller bleeds.
Trauma
Trauma is less common in older pets, but may occur due to fall or accidently injuries (e g. Backed over in driveway). Similar to older people, elderly pets will recover from trauma, but it may be that the recovery time is a bit longer than a young pet. Additionally, it may be that co-morbidities affect anesthesia or even the owner’s goals on proceeding. For example, a 14-year Labrador with severe arthritis in all 4 legs may have much more difficulty and require increased nursing care to recover from pelvic fractures than a 1-year Labrador. Additionally, it is possible that any injuries that originally were considered trauma could represent neoplasia (such as the fractured leg from a fall from a short distance.
Summary
1) Geriatric pets should be evaluated on emergency with any concerns.
2)Urinary tract infection in older pet may result in systemic signs of weakness or frailty.
3) Chronological age is less important that physiological age.
4) Treatment of senior pets is often very rewarding and age alone should never be a reason not to pursue therapy if otherwise indicated.
60
Further reading
1) Hua J, Hoummady S, Muller C, et al. Assessment of frailty in aged dogs. Am J Vet Res. 2016 Dec;77(12):1357-1365.
2) Relford R, Robertson J, Clements C.Symmetric Dimethylarginine: Improving the Diagnosis and Staging of Chronic Kidney Disease in Small Animals.Vet Clin North Am Small Anim Pract. 2016 Nov;46(6):941-60.
3) Smith KF, Quinn RL, Rahilly LJ.Biomarkers for differentiation of causes of respiratory distress in dogs and cats: Part 1 Cardiac diseases and pulmonary hypertension.J Vet Emerg Crit Care (San Antonio). 2015 May-Jun;25(3):311-29.
4) Streeter EM, Rozanski EA, Laforcade-Buress Ad, Freeman LM, Rush JE.Evaluation of vehicular trauma in dogs: 239 cases (January-December 2001).J Am Vet Med Assoc. 2009 Aug 15;235(4):405-8. doi: 10.2460/javma.235.4.405.
61
Feline Trauma:
How Are They Different?
62
Feline Trauma: How Are They Different?
Elizabeth Rozanski, DVM, DACVECC, DACVIM Tufts University School of Veterinary Medicine
Trauma can be divided loosely into blunt and penetrating trauma, with blunt trauma including motor vehicle accidents and penetrating trauma most commonly including bite wounds. While some cats live entirely indoors, others are live a combination of indoors and outdoors, others primarily outside. As veterinarians, it is wise to advise owners that the risk of trauma is greater outdoors, and that if possible cats should be kept indoors. It is also helpful to the bird and local small mammal population to have cats remain indoors. However, not all owners or all cats are willing to follow this advice! Additionally, cats may easily slip out an open door or window, or be injured at home by dogs, children or household accidents Cats should be microchipped to improve the likelihood of finding their families.
After traumatic accidents, cats are more likely to hide and to not show evidence of their injuries. Cats are often found a few hours to a few days after an injury. Due to their smaller body size, blunt trauma, like HBC, is apparently more likely to result in either head trauma or pelvic fractures as trauma to the chest or abdomen is likely to result in death.
Head trauma
The most common triad of injuries in head trauma is a damaged eye or eyes, maxillary fracture, and mandibular fracture. Some cats, but less than guessed, also have traumatic brain injury with altered mentation. Cats will commonly present with increased respiratory rate and effort; this may be from concurrent pneumothorax and pulmonary contusions, or may be due to skull fractures resulting in open mouth breathing. Open mouth breathing results in drying of the secretions (including blood) in the mouth, and this can contribute to apparent respiratory distress.
Treatment of these cats is supportive. The first step may to be to encourage the family to give the affected kitty a bit of time. Facial trauma looks dramatic, particularly proptosis, and occasionally the knee-jerk response is to request euthanasia. Most clients can be convinced to continue treatment and most cats will recover well. The next step is to identify what can be repaired in house and what might require referral and /or advanced imaging. The best approach is what is decided between the primary care veterinarian and the cat’s family and will vary regionally and between practices.
Skull films or CT scanning may be helpful to better characterize the injuries. CT scanning is MUCH better than Skull films to evaluate the bony characteristics, due to superimposition of bones around the skull. However, the main question that needs to be answered is “What is the occlusion”- meaning does the jaw close normally and can it be pushed closed with good occlusion of the maxilla and mandible. If the jaw can be closed, but stays open on its own, often this will resolve as the swelling decreases. The most common fracture is a symphaseal fracture of the mandible, this fracture can easily be repaired in most practices that have access to a 14 or 16 ga needle, some wire and a wire twister or needle driver! However, other fractures, such as mandibular body fractures, may require more complex surgery to return normal alignment. The TMJ may also be dislocated or fractured. A dislocation may be repaired using the “pencil trick”,
63
which involves placing a pencil or wooden dowel in the mouth (like a horse bit) perpendicular to midline and as far caudal as possible. Then the mouth is pushed as closed as possible, and this will reduce the luxation. If there is a fracture, this will not be effective. Maxillary fractures are rarely surgical, and require rest and soft food to heal. In some cases of multiple severe fractures, surgical repair is very challenging, and occasionally you can potentially treat these cats by simple supportive care and then after healing, pull any teeth that are preventing normal occlusion.
Enucleation can be performed for severely injured/blind eyes, or a temporary tarsorrhaphy may be performed if the eye appears like it may be salvaged. In almost all cats with injuries more involved than a simple fracture that can be wired, placement of an e-tube at the time of surgery is advised. Most cats will begin eating voluntarily within 7-14 days from the time of the accident; however, an e-tube will remove the fear of the cat not eating, and also make medication of the cat much easier, as it is far easier to administer liquid medicine via an e-tube than to try to pill a cat with a painful mouth.
Pelvic fractures
Pelvic fractures are also quite common in cats. Fractures are considered surgical if they affect a weight-bearing surface or if the pelvic canal is collapsed. Cats will recover more quickly with orthopedic repair, but cage rest will also permit recovery in most cats. The decision to repair the fractures surgically should be based on a discussion between the cat’s owner and the primary care veterinarian.
Bite wounds
Bite wounds are seen frequently in cats, and may be divided into bite wound from other cats, which are typically not deep, but may abscess or rarely result in a pyothorax and bite wound from dogs, which may be immediately life-threatening. Recall that most bite wound are much worse under the surface than they first appear, and wounds from large dogs typically have four puncture wounds from the canine teeth. Wounds should be carefully explored, and equipment and supplies to enter body cavities readily available. The rabies vaccination status of the patient should be confirmed. Other animal-animal interactions may also result in trauma.
Blood transfusions
In most cats with severe trauma, anemia develops quickly in association with blood loss, sampling and fluid therapy. In particular, recall that cats can lose a fair bit of blood associated with pelvic fractures, and transfusions may be required during recovery. Cat have pre-formed antibiotics against foreign blood types, and care should be taken to type and/or cross-match cats prior to transfusions.
Occult cardiomyopathy
Cats, particularly large male cats who are more prone to trauma, may be similarly prone to hypertrophic cardiomyopathy, which may complicate recovery. Auscultation provides little useful information, but a gallop should be considered evidence of cardiac disease. Cardiac enlargement may be visualized on routine thoracic radiographs, but may be absent as well. Careful monitoring is advised if there is any inkling of heart disease, and echocardiography or NT pro-BNP assessment may prove useful in higher risk cats.
64
Diaphragmatic hernia
DH may occur in cats, particularly those with roll-over injuries. Similar to dogs, DHs should be repaired as soon as practical. Chronic DH are associated with a higher rate of complications, including death from re-expansion pulmonary edema.

Un-owned/Found cats
In ER practice, unknown/stray cats may be presented from time to time by Good Samaritans; it is reasonable to have a practice policy and arrangement with local animal control to help care for these cats. Owned cats can travel some distance, and stabilization therapy is warranted.
Figure 1. A cat with a diaphragmatic hernia found incidentally after routine neuter. The cat had been apparently injured years before and recently adopted.
65
The Acute Abdomen
66
The Acute Abdomen
Elizabeth Rozanski, DVM, DACVIM (SAIM), DACVECC Tufts University School of Veterinary Medicine
An “acute abdomen” is defined as sudden abdominal pain or signs of gastrointestinal upset of an unidentified cause. Any patient presenting with signs of abdominal distress should be promptly evaluated, with a specific goal of determining in the patient has a surgical disease, such as an intestinal obstruction or peritonitis. Ab-dominal signs may be caused by gastrointestinal disease, or extragastrointestinal disease, such as urogenital, splenic mass or torsion, or even musculoskeletal disease. Dogs with pericardial effusion commonly vomit 24- 48 hours prior to presentation with signs of cardiovascular collapse. Some clinicians considered pancreatitis or hepatic disease as extension of gastrointestinal disease while other consider them a separate entity. Many animals with acute gastrointestinal signs will respond rapidly to supportive care, often without specific diagnosis being made. The purpose of this discussion is to review the diagnostic and therapeutic approach to the assessment of the patient presenting with acute abdominal signs.
Initial Assessment
The initial assessment of the dog or cat presented for abdominal pain and/or vomiting and diarrhea should include a quiet assessment of the stability of the major body systems, including the heart, brain, and lungs. Specifically, dogs should be assessed for signs of hypovolemic shock including tachycardia (>160 bpm), weak pulses, labored respiration, or dull mentation. Detection of shock, or possible shock, should be promptly as- sessed and treated. Abdominal pain should be assessed, and if possible localized. In chondrodystrophic dogs, such as dachshunds, back pain masquerading as abdominal pain should be excluded.
Cats are often harder to assess, but similar evaluation for hypovolemia should be made. Additionally, in all male cats, the potential of urinary obstruction should be excluded. Feline aortic thromboembolism (“saddle thrombus”) may present with severe pain, but it is generally quite straight-forward to identify clinically on examination.
If patients are perceived to be unstable, prompt therapy should be initiated to improve the patient’s cardio- vascular status, include administration of intravenous fluid boluses as well as antibiotics, and possibly analge- sics. In stable patients, a more complete physical examination may be completed prior to further diagnostics or treatment.
Other important historical considerations include the age, sex and breed of the patient, as well as any past pertinent history, with a specific focus on gastrointestinal signs. Some dogs may be prone to ingestion of foreign bodies, even as they mature. Vaccination status and/or exposure to potential sick dogs should be investigated. Normal diet, including routine exposure to raw meats, should be evaluated as well as any potential dietary indiscretions such as eating garbage.
The duration and progression of clinical signs should be reviewed, as well as any home therapies. For vomiting patients, pertinent questions include confirmation of vomiting rather that regurgitation, and establishment of any potential useful characteristics of the vomitus, such as blood, bile or foreign objects. For animals with diarrhea, useful questions include the presence of urgency, straining, or bloody, mucousy, or melenic feces.
67
Following a complete history and physical examination, a recommendation should be made to the client sur- rounding further diagnostics or therapy. In animals with a reassuring physical examination, and uncomplicated history, simple supportive care may be adequate, such as an antiemetic and bland diet. However, in many cases, further diagnostic and therapies are indicated.
Diagnostic Testing
Diagnostic testing includes imaging and laboratory testing, with a focus on ruling out surgical disease, and extra-gastrointestinal causes of acute abdominal signs. In many emergency rooms, focused abdominal sonography (POCUS) has emerged as an indispensable tool. Focused sonography is useful for detecting free fluid, which may be promptly sampled, and subsequently evaluated to establish a diagnosis of hemorrhage, sepsis, neoplasia or urinary rupture. Hemorrhage is identified by gross inspection of the fluid, as well as determination of the spun hematocrit. Additionally, spontaneous hemoperitoneum will not clot. Sepsis may be con- firmed by the microscopic identification of intracellular bacteria within neutrophils and strongly suspected by the presence of a glucose or lactate gradient in the abdominal effusion, with an abdominal effusion glucose of 1.1 mmol/l or more lower than the peripheral blood sample or lactate of 2.0 mmol/l higher than peripheral blood. Neoplasia may be confirmed by the presence of neoplastic cells in the effusion, although it is important to recognize that reactive mesothelial cells may be difficult to distinguish from neoplastic cells. Urinary rupture is suspected by the presence of an elevated creatinine and potassium in relation to the peripheral blood and confirmed by a contrast study or exploratory surgery.
Diagnostic peritoneal lavage (DPL) is occasionally referred to in older literature as a technique to retrieve abdominal effusion for diagnostic testing. Focused sonography has largely replaced DPL although it remains of historical interest and may be performed if sonography is not promptly available.
Abdominal radiography is a useful diagnostic modality for evaluating the intra- abdominal structures in dogs and cats with signs of acute abdominal disease. The abdominal structures should be evaluated in a systemic fashion, with a focus on the gastrointestinal tract, as well as the size and shape of the liver, kidney, urinary bladder and reproductive tract. Identification of obstruction, mass or mass-effect or free intra- abdominal air should prompt surgical exploration.
If abdominal radiographs and focused sonography do not identify a clear cause of the acute abdominal signs, a complete abdominal ultrasound may be performed. Some clinicians elect to by-pass abdominal radiography in favor of a complete abdominal ultrasound; the utility of this approach depends on the skills of the ultra-sonographer and the patient assessment by the clinician. Other forms of abdominal imaging, included computed tomography or magnetic resonance imaging, are uncommonly performed in veterinary medicine at this point in time. Some diagnostic imaging specialist favor CT scanning for larger dogs, especial deep-chested or uncooperative dogs.
Laboratory testing is also indicated in dogs and cats with acute abdominal signs and may include point of care testing, as well as more specialized testing. Point of care testing includes determination of the spun hematocrit and total protein, and determination of blood glucose and lactate. Hemoconcentration will be reflected by an increased spun hematocrit, occasionally in excessive of 60%. Dehydrated patients may also have an elevated total protein, often greater than 8.0 gm/dl although with simultaneous hemorrhage or a protein-losing enteropathy the total protein may also be decreased. Blood glucose is typically within normal limits, although in some cases of diabetic ketoacidosis the presenting complaint
68
is vomiting and weakness. In animals with complicated diabetes, the blood glucose should be severely elevated, typically in excess of 500 mg/dl.
Other laboratory testing that may be pursed included a complete blood count (CBC), biochemical profile, and urinalysis as well as more focused testing such as PLI. Laboratory testing in cases of animals with acute abdominal signs is performed to evaluate the patients for extra-gastrointestinal causes of abdominal signs, as well as to evaluate for any co-morbidities that might complicate care, such as severe electrolyte disturbances, azotemia, liver dysfunction, or leukocyte abnormalities, such as a degenerative left shift. Azotemia may be pre-renal, renal or post-renal in origin.
Evidence of inadequate urine concentration (urine specific gravity < 1.030), is often taken as a confirmation of renal azotemia, it is prudent to recall that therapies such as prednisone or furosemide may impact the concentrating ability of the kidneys. Coagulation testing may be pursed in animals with anemia, evidence of gastrointestinal bleeding or disseminated intravascular coagulation.
Supportive Care
Fluid therapy represents the cornerstone of supportive care for patients with acute abdominal disease. When using treating a patient with fluids, they are many important concepts to consider, these include patient characteristics, underlying disease, hospital or clinic characteristics, and fluid types.
Normal fluid balance in an individual is based upon adequate food and water intake. The reported “maintenance” fluid rates for healthy animals are 40-80 m/kg per day; however, this can vary widely depending up the size of the patient. As a guideline, 2-3 ml/kg/hr is a reasonable IV fluid rate in a patient that is adequately hydrated, but not able to maintain hydration for whatever reason. In animals that are dehydrated, a higher fluid rate will be required to provide for maintenance needs as well as rehydrating them. Animals with excessive fluid losses, including polyuria/polydipsia, vomiting/diarrhea, panting or wound /body cavity exudate will require more fluid support to prevent dehydration and/or hypovolemia.
For animals with acute abdominal signs, it is ESSENTIAL to determine if the patient is hypovolemic, simply dehydrated or both. Hypovolemia with a normal interstitial hydration is typically seen in animals with a pera- cute onset of abdominal pain, such as those patients with gastric dilatation-volvulus (GDV), where despite the presence of intravascular volume depletion, the interstitium is adequately hydrated due to the limited duration of clinical signs. Clinical signs of hypovolemia include tachycardia, pale mucous membranes, weak pulses, quiet mentation and occasionally tachypnea. Biochemically, shock is appreciated by increased lactate (>3 mmol/dl) and increased base deficit. These patients should be prompted treated for shock, with an intravenous fluid bolus of 45-90 ml/kg of crystalloids. Fluid boluses should be repeated until the cardiovascular status improves.
In animals with simple dehydration, the cardiovascular parameters remain normal, but the patient has evidence of volume loss. Dehydration is appreciated clinically by dry mucous membranes (if not panting or salivating heavily), decreased skin turgor, and progressively by sunken eyes and tachycardia and collapse. Older cats, in particular, often feel dehydrated even when normal, and young puppies may have good skin turgor de- spite have marked dehydration. If dehydration progresses, a patient may also become hypovolemic. A dehydrated animal that is also hypovolemic should be treated for hypovolemia first, and then have the dehydration corrected.
69
In treated dehydration, the goal is to replace fluid deficit, provide for maintenance needs, and to support any potential on-going losses. Calculating the percentage dehydration is required in determining a fluid rate, so while there are inherent flaws in doing so, it is helpful clinically to pick a number, such as 8% as outline in the chart. The crystalloid dose is calculated by multiplying the weight in kilos by the percentage dehydration. For example, a 20 kg (44 #) dog that is assessed to by 8% dehydration would require the provision of 20 x 0.08= 1.6 kg (or 1600 ml) fluids in order to rehydrate the dog. Importantly fluid therapy needs to provide for on- going losses as well as normal maintenance needs in order to keep the patient from re- dehydrating. In this case, an 20 kg dog that was 8% dehydrated, would need for normal maintenance needs, approximately 60 ml/kg per day (or 1200 ml) and might require an additional 400 ml for on-going excessive losses (e.g., diar- rhea). This patient would then receive 3200 ml of fluid per day (1600 ml dehydration + 1200 ml maintenance + 400 ml on-going losses) or a total of 133 ml/hr. Practically, the clinician might set the fluid rate at 130 or 153 ml/hr.
Key point
Is the situation surgical?
70






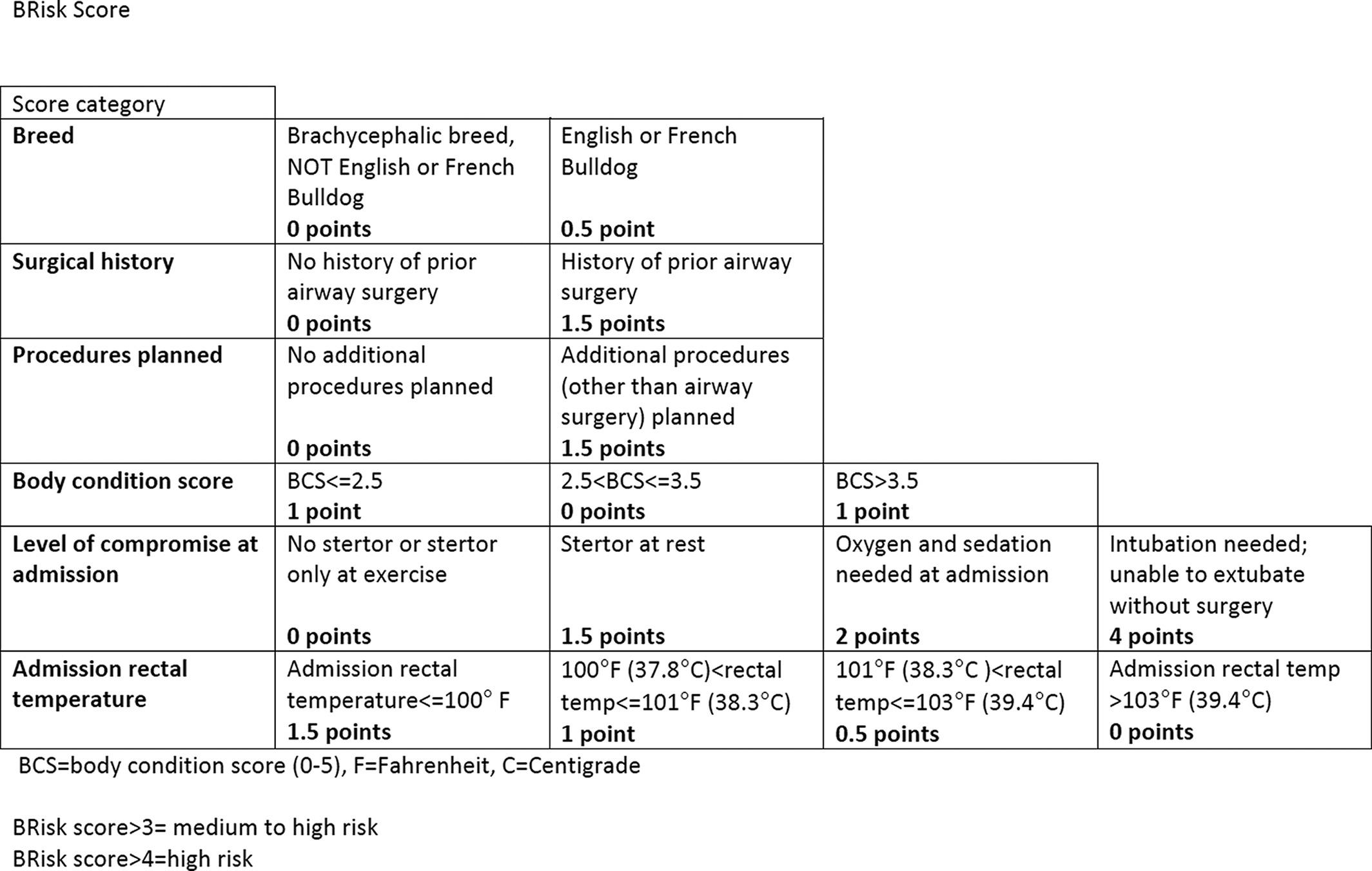
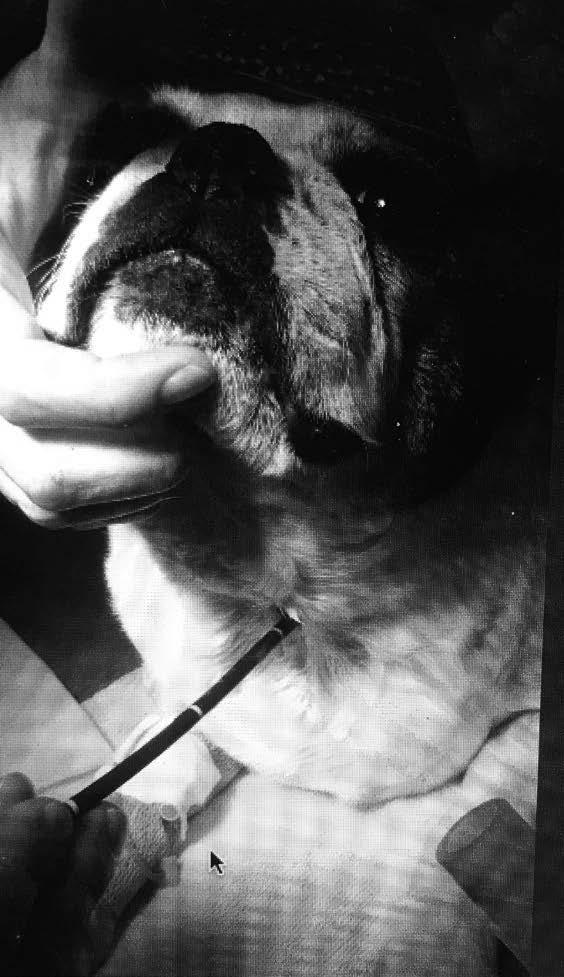
 Figure 1
Figure 1